Expert opinion on priority risk groups for influenza vaccination
This paper identifies and describes population groups at increased risk for severe outcomes of influenza (“risk groups”) and advocates vaccination for two major groups, namely a) persons in the older age group, usually 65 years and older; and b) persons with chronic medical conditions.
Executive summary
At the request of the European Commission, ECDC has conducted a scientific public health review concerning influenza risk groups* and other groups that are offered immunisation against seasonal influenza in Europe. The specific objectives of this study were:
- to describe the risk groups recommended for immunisation in the EU/EEA countries, along with details of other groups for which immunisation is offered;
- to summarise the supporting evidence for the risk groups that are recommended for vaccination;
- to suggest a prioritisation of risk groups in the EU, based on transparent criteria;
- to broadly estimate the number of people in EU countries in priority risk groups; and
- to identify areas for further work, including research and development.
The descriptions of the influenza risk groups and the other groups to whom immunisation is currently offered came from a survey conducted in 2008 by the VENICE project working in conjunction with ECDC. According to the criteria developed by ECDC/VENICE, risk groups should be well-defined groups shown to be more likely to develop severe disease than others. In addition, there should be published evidence that their risk of becoming infected was reduced by immunisation. On the first criterion, the work was hampered by the fact that currently no routine surveillance is conducted in Europe for severe influenza-associated morbidity and mortality. Occupational health criteria (primarily immunising health workers) without demonstrated benefit to patients were noted but given a lower weight — with the exception of one group of workers, those caring for elderly people in residential settings where there is good evidence of this protecting patients. Finally, the degree of consensus among EU countries was noted.
The analysis of literature indicates that there are two risk groups where routine annual immunisation with seasonal influenza vaccine is justifiable on scientific and public health grounds in Europe.
These are:
- older age groups, usually 65 years and older; and
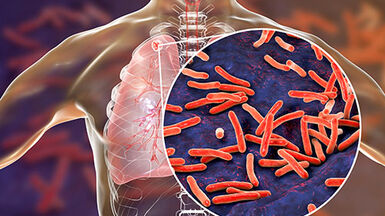
- people with chronic medical conditions, particularly diseases in the following categories:
- chronic respiratory diseases;
- chronic cardiovascular diseases;
- chronic metabolic disorders;
- chronic renal and hepatic diseases;
- persons with deficient immunity (congenital or acquired);
- young people taking long-term salicylate therapy; and − persons with conditions which compromise respiratory function.
These are also the only risk groups for which there is consensus across European Union countries. The exact age definition of the elderly age group is somewhat arbitrary (above 64 years, above 59 years, etc.) and a few countries already depart from the over-64-years criterion, depending on national circumstances and analyses.
Some good arguments exist for offering immunisation to two other risk groups: pregnant women and children (variously defined as ‘below age two’ or ‘below age five’). However, for both groups there is only limited information available in Europe, both on risk and on effectiveness, and there is as of yet no European consensus. Data are insufficient for these two groups to be identified as risk groups at the EU level. As more information and data become available, these groups will have to be re-evaluated. It is especially important that data on the impact of immunisation in these groups are collected so that a consensus can be reached after further evaluations.
There are also groups for which immunisation is often offered but that are not in risk groups and for which there is no strong public health case. For example, there is considerable EU consensus that all health-care workers with patient contact should be immunised for occupational health reasons (protecting the workers). There is strong trial-based evidence that immunising those caring for elderly people in residential homes indirectly benefits the patients, protecting them against severe outcomes of influenza infection. However, it is notable that most health workers in Europe decline such offers of immunisation. There is no good evidence of benefits from offering immunisation to people sharing households with people in the two main risks groups.
Broad estimates are made as to the numbers and percentages of people who belong to the two main risk groups in EU countries. This study applied one method that suggested that EU countries currently need to immunise about 25% of their populations every year as they belong to at least one of the two major risk groups. Other national estimates have come up with similar percentages. The national range is from 19% to 28%, depending on the percentage of elderly people in the population in each country. The EU total is estimated to be around 125 million people, split two-thirds (around 84 million people who are 65 years or over) to one-third (around 41 million younger persons with chronic illness). These figures will rise inexorably over time because of aging populations and the success of modern medicine in permitting people with chronic illness to live longer productive lives.
This study recommends a number of priorities for European development and research:
- surveillance development: routine surveillance for severe manifestations of influenza in Europe (hospitalisations and death);
- routine monitoring of the effectiveness of influenza vaccination, especially in reducing the risk of severe disease and death from influenza;
- estimation of the burden of disease from influenza in pregnant women and children, and evaluation of the impact of immunising pregnant women and children of all ages in Europe;
- further investigations to demonstrate whether or not immunisation of health-care staff and household members reduces risk in vulnerable people in the two main risk groups;
- development of projects for stronger promotion of influenza immunisation among health-care workers, both for their own benefit and for that of their patients;
- specific investigations as to whether or not there are higher levels of risk of severe disease from influenza infection in HIV-infected persons in Europe and similar studies for other more common conditions such as mild asthma;
- health impact and health economic studies concerning influenza immunisation, e.g. on persons above the threshold age for immunisation, acknowledging that different countries need to set their own age thresholds;
- investigation of the impact of across-the-board immunisations to determine any indirect benefit from reducing overall levels of transmission.
Download

Read more on the ECDC website
Risk groups for severe influenza
Some people are at high risk of serious complications as a result of influenza, some of which can be life-threatening and result in death.
Immunisation information systems in the EU and EEA
This report presents the findings of a survey conducted by ECDC across EU/EEA countries that assessed the level of implementation of IIS and their functionalities, as well as the challenges encountered during the design and implementation.
European Immunization Week campaign
European Immunization Week (EIW) is celebrated across the European Region every April to raise awareness of the importance of immunisation for people’s health and well-being.
Latest updates on influenza vaccination
Featured
Expert opinions
Expert opinions are scientific views or comments by a group of designated experts based on a review of scientific evidence and/or expert opinion.