Antimicrobial resistance in the EU/EEA (EARS-Net) - Annual epidemiological report for 2022
In 2022, for the first time, all European Union/European Economic Area (EU/EEA) countries reported data to the European Antimicrobial Resistance Surveillance Network (EARS-Net).
Executive summary
- In 2022, for the first time, all European Union/European Economic Area (EU/EEA) countries reported data to the European Antimicrobial Resistance Surveillance Network (EARS-Net).
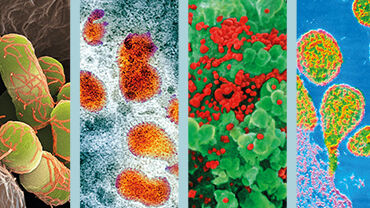
- Compared to 2021, the total number of reported isolates increased from 366 794 to 392 602. The most commonly reported bacterial species in 2022 were Escherichia coli (39.2%), followed by Staphylococcus aureus (22.1%), Klebsiella pneumoniae (12.3%), Enterococcus faecalis (8.2%), Pseudomonas aeruginosa (6.1%), Enterococcus faecium (5.9%), Streptococcus pneumoniae (3.7%) and Acinetobacter spp. (2.5%). This ranking differed from 2021, with P. aeruginosa and S. pneumoniae one rank higher in 2022.
- On 13 June 2023, the Council of the EU adopted a Recommendation on stepping up EU actions to combat antimicrobial resistance (AMR) in a One Health approach (2023/C 220/01), which recommends targets to be achieved in the EU by 2030. The targets include three AMR targets to reduce the total EU incidence of bloodstream infections with meticillin-resistant S. aureus (MRSA), third-generation cephalosporin-resistant E. coli and carbapenem-resistant K. pneumoniae, by 15%, 10% and 5%, respectively, by 2030 against the baseline year 2019. While the EU incidence of bloodstream infections with both MRSA and third-generation cephalosporin-resistant E. coli showed a favourable decreasing trend between 2019 and 2022, the EU incidence of carbapenem-resistant K. pneumoniae increased by almost 50%.
- AMR percentages remain high in the EU/EEA and there are specific AMR issues that are a concern, such as the continuous increase in carbapenem-resistant K. pneumoniae (10.9% in 2022) and vancomycin-resistant E. faecium (17.6% in 2022).
- Of note for 2022 were the decreases in the EU/EEA population-weighted mean AMR percentages for Acinetobacter spp. compared to 2021, and a significantly increasing trend for the EU/EEA population-weighted mean percentage of macrolide resistance and penicillin non-wild-type, including combined resistance in S. pneumoniae during the period 2018−2022.
- The AMR situation reported by EU/EEA countries varied widely depending on the bacterial species, antimicrobial group and geographical region. In general, the lowest AMR percentages and estimated incidence of bloodstream infections with resistant bacteria were reported by countries in the north of Europe and the highest by countries in the south and east of Europe.
- For each bacterial species, country-specific information on estimated incidence of bloodstream infections for the EU targets, data availability, and age group, sex and intensive care unit (ICU) patient percentages is available in the country profiles. Results by age group and sex for specific AMR phenotypes are available in European Centre for Disease Prevention and Control (ECDC) Surveillance Atlas of Infectious Diseases.