Epidemiological update: Middle East respiratory syndrome coronavirus (MERS-CoV), 29 May 2015
Epidemiological update of MERS-CoV from the Middle East and the rest of the world
Recent developments
South Korea
On 20 May 2015, the South Korean Centers for Disease Control and Prevention reported a case of Middle East respiratory syndrome coronavirus (MERS-CoV) in a 68-year-old man, with recent travel history to Middle East. According to WHO, the man had the following travel history:
- 18-29 April, Bahrain;
- 29-30 April, United Arab Emirates;
- 30 April to 1 May, Bahrain;
- 1-2 May, the Kingdom of Saudi Arabia;
- 2 May, Bahrain; and
- 2-3 May, Qatar.
The case arrived at Korea’s Incheon International airport via Qatar on 4 May, while being asymptomatic. On 11 May, he developed cough and fever and sought medical care at an outpatient clinic between 12 and 15 May. He was hospitalised on 15 May, discharged on 17 May and readmitted same evening in another hospital after presenting to the emergency department. On 20 May he tested positive for MERS-CoV and was transferred to the nationally designated treatment facility for isolation. The patient has no history of exposure to known risk factors in the 14 days prior to detection. Investigation of the source of infection is ongoing. [1]
As of 30 May, the index case has resulted in eleven secondary cases:
- One patients sharing his room and four patients admitted in the same ward;
- Three healthcare workers having cared for the index case;
- Three among close family members: the wife of the index case, and the son and daughter of a patient admitted in the same ward.
Onset dates range from 11 May for the index case, until 28 May for the two most recent nosocomial cases, according to the Korean Centers for Disease Prevention and Control.
The son of the patient admitted in the same ward travelled to Hong Kong, Guangdong province, China, on 26 May 2015. He was admitted and isolated in a hospital in Hong Kong on 27 May 2015. This patient was confirmed positive for MERS-CoV infection on 29 May. [2]
United Arab Emirates
The United Arab Emirates have reported in May 2015 two asymptomatic cases found through enhanced surveillance. According to WHO, both cases had a history of contact with MERS-CoV infected camels imported from Oman. The United Arab Emirates have reported 76 cases of MERS-CoV since 13 July 2013. Twenty-nine of the 76 cases were healthcare workers.
Qatar
Since the last rapid risk assessment on 7 March 2015, Qatar has reported three additional cases. All cases were male. One of the cases had frequent contact with camels.
Saudi Arabia
Since the last rapid risk assessment on 7 March 2015, Saudi Arabia has reported 72 additional cases and 40 deaths. Of the 72 cases, 78% (n=56) were male. The average age for 72 cases was 53 years, ranging from 20 to 93 years. Twenty-one of the 72 cases were classified as having contact to a confirmed case either in the community or hospital. Five of the 72 cases were healthcare workers. Eight of the 72 cases reported animal contact and seven reported to have drank camel milk.
Worldwide situation
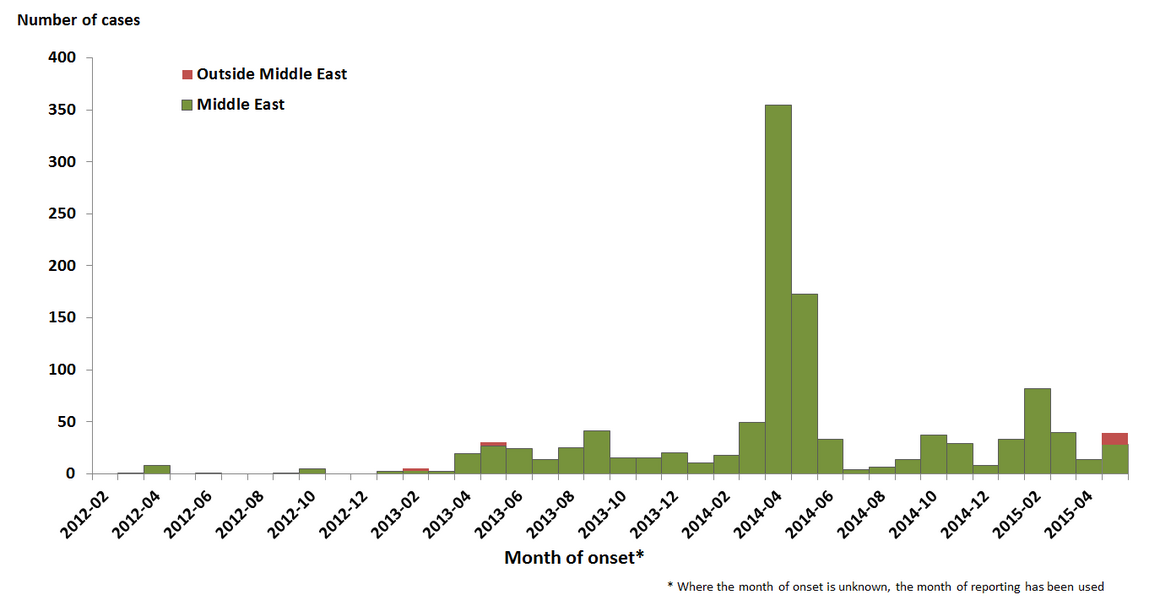
Since April 2012 and as of 30 May 2015, 1 172 cases (including 479 deaths) of MERS-CoV have been reported by health authorities worldwide (Figure 1).
Figure 1. Distribution of confirmed cases of MERS-CoV by month and probable place of infection, March 2012– 30 May 2015 (n=1 172)
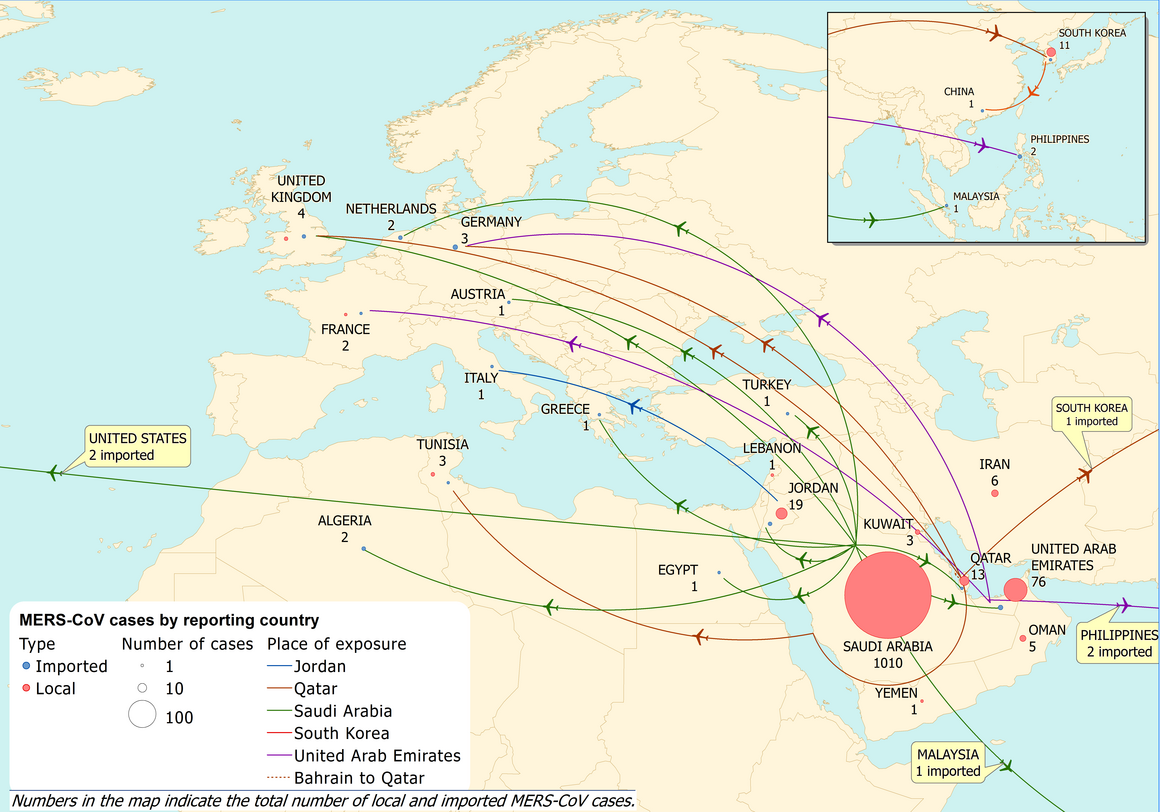
Geographical distribution Most of the cases have occurred in the Middle East (Saudi Arabia, United Arab Emirates, Qatar, Jordan, Oman, Kuwait, Egypt, Yemen, Lebanon and Iran) (Table2).
Table 2. Confirmed cases and deaths, by country of reporting, March 2012 – 30 May 2015
| Reporting country | Cases | Deaths |
|---|---|---|
| Middle East | | |
| Saudi Arabia | 1 010 | 442 |
| United Arab Emirates | 76 | 10 |
| Qatar | 13 | 4 |
| Jordan | 19 | 6 |
| Oman | 5 | 3 |
| Kuwait | 3 | 1 |
| Yemen | 1 | 1 |
| Lebanon | 1 | 0 |
| Iran | 6 | 2 |
Europe |
||
| Turkey | 1 | 1 |
| Austria | 1 | 0 |
| United Kingdom | 4 | 3 |
| Germany | 3 | 1 |
| France | 2 | 1 |
| Italy | 1 | 0 |
| Greece | 1 | 1 |
| Netherlands | 2 | 0 |
| Rest of the world | | |
| Tunisia | 3 | 1 |
| Algeria | 2 | 1 |
| Malaysia | 1 | 1 |
| Philippines | 2 | 0 |
| Republic of Korea | 11 | 0 |
| United States of America | 2 | 0 |
| People's Republic of China | 1 | 0 |
| Cumulative number | 1 172 | 479 |
All cases reported from outside the Middle East have a recent travel history to the Middle East or contact with a case who has a travel history to the Middle East (Figure 2).
Figure 2. Geographical distribution of confirmed MERS-CoV cases and place of probable infection, as of 29 May 2015 (n=1 172)
ConclusionThe importation of a case of MERS-CoV to a third country is not unexpected and has happened in the past. On several occasions, notably in France and in the UK, it has resulted in secondary transmission among patients and healthcare workers in contact with the imported cases, as well as among close relatives of cases. However, clusters of this size have not been observed so far outside of the Arabian Peninsula. WHO indicates that there is currently no indication that the virus behaves differently than in other instances in the past and that there is no indication of sustained transmission from person to person. It is the first time that an imported case results in a secondary transmission affecting another country.
ECDC’s conclusion continues to be that the MERS-CoV outbreak poses a low risk to the EU. Because of the continued risk case importation to Europe after exposure in the Middle East, international surveillance for MERS-CoV cases remains essential.
Although sustained human-to-human transmission is unlikely, secondary transmission in unprotected close contacts, including healthcare settings, remains possible, as currently seen in South Korea.
An overview of MERS-CoV infection is presented in an ECDC fact sheet [3], which also provides a detailed overview of measures to be taken by health professionals for case management and treatment.
References1. World Health Organization. Middle East respiratory syndrome coronavirus (MERS-CoV) – Republic of Korea [Internet]. 2015 [updated 24 May 2015]. Available from: http://www.who.int/csr/don/24-may-2015-mers-korea/en/.2. Korean Centers for Disease Control and Prevention. MERS-CoV overview [Internet]. 2015 [updated 28 May 2015]. Available from: http://www.mw.go.kr/front_new/al/sal0301vw.jspPAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=322602.3. European Centre for Disease Prevention and Control. Factsheet for health professionals 2014. Available from: http://www.ecdc.europa.eu/en/healthtopics/coronavirus-infections/mers-factsheet/Pages/default.aspx.4. World Health Organization. WHO statement on the Eighth Meeting of the IHR Emergency Committee regarding MERS-CoV [Internet]. Geneva: WHO; 2015. Statement]. Available from: http://www.who.int/mediacentre/news/statements/2015/8th-mers-emergency-committee/en/.5. European Centre for Disease Prevention and Control. Preparedness planning for respiratory viruses in EU Member States – Three case studies on MERS preparedness in the EU. Stockholm: ECDC; 2015. Available from: http://www.ecdc.europa.eu/en/publications/Publications/Preparedness%20planning%20against%20respiratory%20viruses%20-%20final.pdf.