Lice (Phthiraptera) - Factsheet for health professionals
Disclaimer: the information contained in this fact sheet is intended for the purpose of general information and should not substitute individual expert advice from healthcare professionals.
Hazard associated with lice species
Current issues
Lice (Phthiraptera) are a very diverse group of insects, exclusively adapted to parasitism. Several thousand species have been described to date [1]. Their body is flattened dorso-ventrally, they are wingless, relatively small in size (0.4−10 mm in length) and have a hemimetabolic (incomplete metamorphosis) life cycle, comprising adults (males and females), eggs (known as nits) and three nymphal stages [2,3]. Lice generally have a high host-specificity, and within a host species there is sometimes also a specificity to certain body regions. They are widely distributed across the globe. Lice can be divided into two main groups: sucking lice (Anoplura) and chewing lice (Mallophaga). All active stages of lice are parasitic in warm-blooded vertebrates (birds and mammals) [3]. The two groups differ in their feeding habits, with Mallophaga feeding on skin and skin products and Anoplura generally feeding on blood. The groups can be easily differentiated morphologically. Anoplura are an important pest and disease vector affecting both public and veterinary health. Mallophaga are important pest species for animals, but not for humans.
Invasive species/global dispersion
Most lice with public health and veterinary relevance have a global distribution, as they are associated with hosts that are also widely dispersed. Their global distribution is mediated by humans via tourism, transport, and the trade of pets and livestock. A particularly interesting louse is Heterodoxus spiniger which was originally a parasite of marsupials in Australia, later switched to dingoes, and from these moved to domestic dogs. The species is now spread worldwide in various carnivores, including domestic dogs [3].
Ecological plasticity
All active stages of lice are obligatory parasites, but with a relatively high host-specificity.
Biting and disease risk
Only those sucking lice with humans as their host species are of relevance to public health. Apart from causing nuisance, human body lice are also important vectors of diseases.
Anoplura
Anoplura are important parasites of both humans and animals. In humans, louse infestation is known as pediculosis if caused by head or body lice, and as pthiriasis if caused by pubic lice. Pediculosis is a contagious parasitic infestation, transmitted from human-to-human by close contact or, in body lice, via infested clothes or bed linen. The most common louse infestation in humans is pediculosis capitis (caused by Pediculus humanus capitis), particularly affecting school children between three and 11 years, and clinically manifesting as scalp pruritus [4]. It is estimated that head lice infest more than 100 million people worldwide [5]. Pediculosis corporis (caused by Pediculus humanus humanus) is a major public health concern, mainly occurring in crowded human communities, such as refugee camps or shelters for homeless, where hygiene is poor and clothes or linen are not washed regularly [4]. At homeless shelters in Europe, the prevalence of body lice can reach over 20% [6]. The clinical signs of body lice infestation include intense pruritus and cutaneous rash, associated with allergy to the bites. In chronic infestations, the skin becomes thickened [5]. Pubic lice, Pthirus pubis, cause pubic pruritus.
Due to their blood feeding behaviour, body lice can transmit a great variety of diseases, such as epidemic typhus (caused by Rickettsia prowazekii), louse-borne relapsing fever (caused by Borrelia recurrentis), or trench fever (caused by Bartonella quintana) [3]. Head lice and pubic lice are not known as vectors of pathogens, but head lice can be involved in mechanical transmission of opportunistic bacteria.
In animals, the presence of sucking lice can cause irritation through the permanent blood feeding. Salivary components induce severe itching which causes skin lesions due to intensive pruritus. Although the amount of blood consumed by each louse is negligible (less than 0.1 mg/meal), high intensity infestations can induce anaemia, mainly in young animals. Other clinical signs may include one or more of the following: alopecia, squamous dermatitis, skin thickening and more or less severe pruritus. At farms with heavily infested animals economic losses can also be incurred as a result of decreased milk and meat production. Due to the direct contact of salivary antigens with the host’s blood, there is a significant immune response to sucking lice, which protects the host after multiple exposures. This is probably the reason why sucking lice are more common in young animals than in adults, at least as regards domestic animals. Various types of hypersensitivity are also known to occur in sucking lice infestations [2]. In domestic animals, sucking lice can also transmit some diseases (see ‘Epidemiology and transmission of pathogens’).
Mallophaga
There are no Mallophaga species that are known parasites of humans. Moreover, as chewing lice are highly host-specific, the species, which are parasitic for animals, will never infest humans, even temporarily. In animals, most of the cases of chewing lice infestation are asymptomatic as the host has various defence mechanisms. These include grooming, moulting, hair or feather loss. Hibernation and hormonal changes of the host can also reduce the load of chewing lice. In some hosts, lice have their own predators, such as fungi or bacteria. In animals with concurrent conditions (weak, inability to stand up, etc.), lack of grooming is associated with high louse densities. The intensity of infestations may also be high in very young or very old animals [3]. Heavy infestations with chewing lice generally induce itching and pruritus, associated with localised alopecia and excoriations [2]. In heavily infested animals, economic loss can be incurred (e.g. decreased milk production and growth or losses associated with inferior hides in the leather industry). Infested sheep tend to rub against hard surfaces and display significant fleece loss [3]. In dogs and cats, skin debris is visible in the fur and pruritus is common. In guinea pigs, the infestations are common when animals are held in large groups (i.e. in pet shops) and can cause severe stress. In poultry, the symptoms are dependent on the phylogenetic louse group. Most members of Amblycera (a group of chewing lice) are able to destroy the quills of feathers. Members of Ischnocera chew parts of the feathers, causing partial feather damage. As in mammals, chewing lice that infest birds can cause mild to moderate pruritus [2]. Due to intense grooming, lice can indirectly cause digestive problems in the host resulting from the formation of hair balls, mainly in cats and calves [3]. Despite limited contact with the host’s blood, there is evidence suggesting the presence of an immune response to chewing lice. Studies in sheep provide evidence of the presence of specific antibodies, T-cell responses and type I and III hypersensitivity reactions which complicate the skin lesions [2]. Chewing lice do not play an important role in pathogen transmission. However, some species (i.e. the chewing lice of carnivores) act as an intermediate host for Dipylidium caninum which is transmitted to dogs and cats via ingestion. Some chewing lice infesting birds are able to transmit avian filariases [2,3].
Geographical distribution
Brief history of spread and European distribution
All lice are co-distributed with their specific host, meaning that species that are parasitic in domestic animals and humans have a global distribution. Their spread probably occurred simultaneously with the colonisation of continents by early humans and their domesticated animals.
Future expansion
It is unlikely that lice will change their geographical distribution in the future, except in situations when infested domestic animals are introduced into lice-free areas (e.g. remote islands).
Entomology
Species name/Classification (selected species): Phthiraptera:
Anoplura: Pediculidae (Pediculus humanus capitis, Pediculus humanus humanus), Pthiridae (Pthirus pubis), Haematopinidae (Haematopinus eurysternus, Haematopinus tuberculatus, Haematopinus asini, Haematopinus suis), Linognathidae (Linognathus vituli, Linognathus ovillus, Linognathus africanus, Linognathus stenopsis, Linognathus setosus).
Mallophaga: Trichodectidae (Bovicola bovis, Bovicola ovis, Bovicola caprae, Bovicola equi, Bovicola breviceps, Trichodectes canis, Felicola subrostratus), Boopiidae (Heterodoxus spiniger), Menoponidae (Menopon gallinae), Philopteridae (Goniocotes gallinae, Columbicola columbae, Anaticola anseris, Anaticola crassicornis).
Common names:
Anoplura: sucking lice.
Pediculus humanus capitis: head louse
Pediculus humanus: body louse
Pthirus pubis: pubic louse or crab louse
Mallophaga: chewing lice.
Morphological characters and similar species
Anoplura
The sucking lice (Anoplura; Greek: ‘anoplos’ = unarmed; ‘ura’ = tail) are ectoparasites of placental mammals, with a worldwide distribution. As opposed to chewing lice, their main feeding behaviour is hematophagous and, as a result, they induce a different pathology and can be important vectors for several medically important pathogens. Sucking lice are less biodiverse than chewing lice as they currently include around 550 species, grouped into 50 genera and 15 families. Of these, only a few are parasitic in humans and domestic animals (Table 1). Most of the general morphological features of sucking lice are similar to those of chewing lice. A notable difference from chewing lice is that the head of a sucking lice is slender and narrower than the thorax. Sucking lice also lack maxillary palps. The mouthparts are adapted for blood feeding and are only visible during feeding. All three thoracic segments are fused, and the thorax appears as one single segment [3]. The antennae are clearly visible and have three to five segments [2].
There is an ongoing debate on the taxonomic status of the human head louse and body louse. They are currently considered to be two subspecies of the same species. A study on the sequence variation of two intergenic spacers in human head and body lice showed that the two subspecies cannot be genetically differentiated and sequence types vary on a bio-geographical basis [7]. However, regardless of their taxonomic status, it is clear that head lice and body lice are different in terms of their relevance to public health.
Mallophaga
The chewing lice (Mallophaga; Greek: ‘mallos’ = wool; ‘phagein’ = eat) are ectoparasites of birds and mammals (marsupial and placental), with a worldwide distribution. They are quite a biodiverse group, with more than 2 600 known species. No species of chewing lice are known to feed on humans. Most of the species are parasitic in wildlife but several are also known from domestic animals and are divided into two main groups of veterinary importance: Amblycera and Ischnocera (Table 2). In both groups the body is flattened dorso-ventrally and the head is generally wider than the first segment of the thorax. The main difference between the two groups of chewing lice is in the morphology of the antennae (four segments in Amblycera, located in a groove lateral to the head; three-to-five segments in Ischnocera, free from the head and clearly visible) and of the maxillary palps (present in Amblycera, absent in Ischnocera) [2,3]. The thorax is usually segmented into two or three parts. The abdomen (which has 11 segments) is elongated and is protected by sclerotised plates which confer a certain rigidity to the body, even when the abdomen is distended. The adult females possess gonopods on the caudal part of the abdomen and these are used to control and glue the eggs to the hair or feathers of the host [3]. As in other hemimetabolic insects, immature stages (nymphs) resemble adults, but are smaller and lack genital structure.
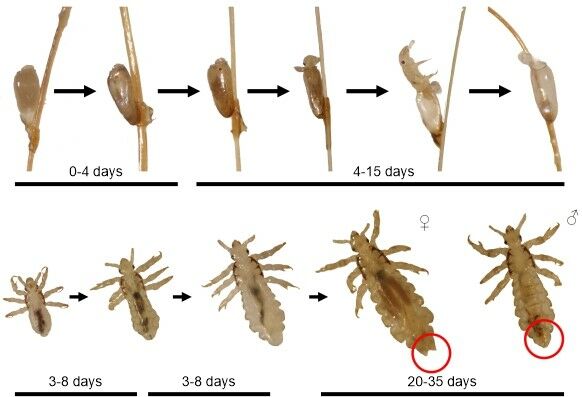
Development and life cycle
The life cycle of sucking and chewing lice is generally similar. Reproduction is sexual and occurs on the host. However, there are a few species which are parthenogenetic, such as B. bovis. Males usually make up around 1−5% of the total adult population on a host. The female lice lay around 0.2−10 eggs per day, which they glue to the hair or feathers. The eggs of the lice are known as nits. The first nymphal stage emerges following an incubation period of 4−15 days. Each of the three nymphal stages, which have the same feeding behaviour as the adults, develop to the next stage in around three to eight days, separated by moulting. The lifespan of adult lice is around 35 days (Figure 1). Although all lice are permanent parasites, some species of chewing lice can survive off-host for several days [3].
Figure 1. Developmental cycle of the human head louse
Most sucking lice cannot survive more than a few hours without a blood meal, hence their limited ability to survive off-host. Survival off-host is generally greater at low temperatures and high humidity. At 26°C and 65% relative humidity (RH), 4% of human body lice die within 24 hours, 20% die within 40 hours, and 84% die within 48 hours [3]. Therefore, head and body lice are generally transmitted from human-to-human as a result of close contact. Occasionally, head lice can also be transmitted via hats, scarves, coats, hair ribbons, combs, brushes, or towels, if the exchange is quick. Body lice can be transmitted through infested clothes or linen. The pubic or crab louse is transmitted during sexual contact.
In domestic and wild mammals, chewing and sucking lice are transmitted by direct contact, including mating or fighting. Another common means of transmission is from mother to offspring during suckling, while in birds, nest sharing plays a crucial role. As some chewing lice can survive off-host, indirect transfer (via the environment) is also possible. Another interesting method of transmission is phoresy - when lice attach to larger hematophagous insects (i.e. flies) and move to other hosts [3].
Feeding behaviour
As their name suggests, sucking lice feed primarily on blood. The sucking is enhanced by the presence of strong oesophageal muscles. Digestion of blood is enhanced by the presence of mutualistic microbiota. Blood ingestion is crucial for the production of eggs [2].
Chewing lice typically feed on various skin products (fur, feathers, skin debris, secretions). However, some species (mainly members of Amblycera) can occasionally feed on blood, after biting into the quills of the feathers. The keratin is digested by endosymbiotic bacteria.
Activity
In the case of humans, body lice live in clothing and their prevalence seems to be higher during winter, associated with lower environmental temperature. However, greater prevalence is also linked to increased humidity and also social factors, such as poverty and poor hygiene which play a role all year round. Body lice are likely to leave a febrile human host and move to healthy individuals, enhancing the efficiency of disease transmission in human populations [8]. Head lice are more commonly diagnosed after school holidays [9]. Seasonal variation has also been described for sucking lice that infect cattle, with higher parasitic loads during winter and spring [2].
There are generally no seasonal differences in the intensity of chewing lice infestations, although in large domestic animals, increases in chewing lice density have been observed during winter [3].
Host preference
Anoplura
All species of domestic mammals have one or several associated sucking lice species. Humans, pigs and rabbits are only infested by sucking lice (i.e. no chewing lice). Sucking lice do not infest birds. Most species are host-specific and some are even body-region specific (Table 1).
Table 1. Sucking lice of medical and veterinary importance (based on [3])
|
Host species |
Louse species |
Family |
|---|---|---|
|
Cattle |
Haematopinus eurysternus Haematopinus quadripertusus Haematopinus tuberculatus |
Haematopinidae |
|
Linognathus vituli Solenopotes capillatus |
Linognathidae |
|
|
Buffalo |
Haematopinus tuberculatus |
Haematopinidae |
|
Sheep |
Linognathus ovillus Linognathus pedalis Linognathus africanus |
Linognathidae |
|
Goat |
Linognathus africanus Linognathus stenopsis |
Linognathidae |
|
Equids |
Haematopinus asini |
Haematopinidae |
|
Swine |
Haematopinus suis |
Haematopinidae |
|
Dog |
Linognathus setosus |
Linognathidae |
|
Rabbit |
Haemodipsus ventricosus |
Polyplacidae |
|
House mouse |
Polyplax serrata |
Polyplacidae |
|
Hoplopleura captiosa |
Hoplopleuridae |
|
|
Rat |
Polyplax spinulosa |
Polyplacidae |
|
Hoplopleura pacifica |
Hoplopleuridae |
|
|
Human |
Pediculus humanus capitis Pediculus humanus humanus |
Pediculidae |
|
Pthirus pubis |
Pthiridae |
Mallophaga
Mallophaga use mammals and birds as hosts (Table 2). Most domestic animal species can act as hosts for chewing lice, notable exceptions being pigs, rabbits and humans. The majority of species are very specific to their host, while others can feed on multiple (but related) host species. Moreover, many species (mainly lice associated with birds) display site specificity (i.e. some species are found only on the head and others only on the body [3]).
Table 2. Representative species of chewing lice in domestic animals (based on [2,3])
|
Host species |
Louse species |
Family |
Group |
|---|---|---|---|
|
Cattle |
Bovicola bovis |
Trichodectidae |
Ischnocera |
|
Sheep |
Bovicola ovis |
Trichodectidae |
Ischnocera |
|
Goat |
Bovicola caprae Bovicola limbatus Bovicola crassipes |
Trichodectidae |
Ischnocera |
|
Horse |
Bovicola equi |
Trichodectidae |
Ischnocera |
|
Donkey |
Bovicola equi asini Bovicola ocellatus |
Trichodectidae |
Ischnocera |
|
South American camelid |
Bovicola breviceps |
Trichodectidae |
Ischnocera |
|
Dog |
Trichodectes canis |
Trichodectidae |
Ischnocera |
|
Heterodoxus spiniger |
Boopiidae |
Amblycera |
|
|
Cat |
Felicola subrostratus |
Trichodectidae |
Ischnocera |
|
Guinea pig |
Gliricola porcelli Gyropus ovalis |
Gyropidae |
Amblycera |
|
Trimenopon hispidum |
Trimenoponidae |
Amblycera |
|
|
Chicken |
Menopon gallinae Menacanthus stramineus |
Menoponidae |
Amblycera |
|
Goniocotes gallinae Goniocotes gigas Goniocotes dissimilis Cuclotogaster heterographus Lipeurus caponis |
Philopteridae |
Ischnocera |
|
|
Turkey |
Menacanthus stramineus |
Menoponidae |
Amblycera |
|
Chelopistes meleagridis |
Philopteridae |
Ischnocera |
|
|
Oxylipeurus polytrapezius |
|||
|
Dove/pigeon |
Hohorstiella lata |
Menoponidae |
Amblycera |
|
Columbicola columbae |
Philopteridae |
Ischnocera |
|
|
Campanulotes compar |
|||
|
Goose |
Anaticola anseris |
Philopteridae |
Ischnocera |
|
Anatoecus icterodes |
|||
|
Trinoton anserinum |
Menoponidae |
Amblycera |
|
|
Duck |
Anaticola crassicornis |
Philopteridae |
Ischnocera |
|
Trinoton querquedulae |
Menoponidae |
Amblycera |
Epidemiology and transmission of pathogens
Lice as vectors of pathogens of public and veterinary health importance
Only the body louse is considered to be a vector of human pathogens. The diseases transmitted by body lice are usually associated with overcrowded and unsanitary conditions where basic hygiene is lacking and regular washing and changing of clothes is not possible.
Epidemic typhus
Epidemic typhus is caused by Rickettsia prowazekii, an obligate gram-negative intracellular coccobacillus transmitted between humans by body lice. Epidemic typhus is an important cause of morbidity and mortality during wars, but otherwise it is a public health issue which mainly affects poor countries [8]. R. prowazekii is known to survive in the lymph nodes or other tissues of humans who recover from epidemic typhus for several years. This enables the pathogen to later reinvade other body tissues to cause a disease known as Brill-Zinsser disease [10]. Information on the bacteraemia is available for laboratory animals in experimental studies [11]. After a blood meal, the pathogen develops in the epithelial cells of the louse midgut from where, after five-to-seven days, they are expelled with the faeces. Mixed with louse faeces, these dry to form a fine black powder which infects small wounds caused by scratching, or by entering the mucous membranes of nose or mouth. There is no vertical transmission of R. prowazekii in lice [3]. The main clinical manifestations in humans include high fever, myalgia, headache, cough and rash. Humans are the main reservoirs but other mammals, such as the flying squirrel (Glaucomys volans), are also known to be natural reservoirs in USA [8]. Epidemic typhus due to R. prowazekii is rarely reported among tourists [12]. Recent outbreaks have been reported in Russia, Burundi, Algeria, and Peru [8]. Epidemic typhus is not present in Europe [13], however imported cases [14] [15] or relapsing forms (known as Brill-Zinsser disease) [16] are sporadically reported. Due to the often-high prevalence of body lice, refugee camps and prisons represent a risk factor for epidemic typhus outbreaks [17]. A R. prowazekii infection can be suspected in travellers and people living in unfavourable hygienic conditions presenting fever, headache and/or rash [13].
Trench fever
The aetiological agent of trench fever is Bartonella quintana, transmitted by the body louse. Human infection most probably occurs through contaminated louse faeces via microlesions following scratching [18]. It typically occurs with general, non-specific symptoms (fever, malaise, headache) but is associated with bacteraemia. Significant outbreaks occurred during the two World Wars, but also later in Poland (1949), Mexico (1954), USSR (1960), and Ethiopia (1964). A recent series of cases was reported in Denver, Colorado in 2020 [18]. Several studies documented high seroprevalence values for B. quintana. In Paris, France, 54% of homeless people with skin conditions were seropositive for B. quintana [19]. In Marseille, France, 14% of the homeless patients who presented with fever at emergency services were seropositive for B. quintana, with an overall seroprevalence in homeless people between 1.8% and 5.3% [20]. Another study from Marseille detected 20% of the body lice collected from homeless people in Marseille to be positive for B. quintana. Bartonella quintana was also detected in head lice from France [21] and various African countries, USA and Nepal [5].
Louse-borne relapsing fever
Louse-borne relapsing fever is caused by the spirochete Borrelia recurrentis, associated with war, famine, refugees, poverty, and poor personal hygiene [22]. Nowadays the disease seems to be confined to eastern and northern Africa. In Europe, it used to be a common disease until the end of the nineteenth century [4] [22]. The main vector is the human body louse, but the agent has also been detected in the head lice of pygmies in Congo, with no evidence of transmission [23]. Humans are the only known reservoirs of infection [22]. After lice are infected, Borrelia recurrentis multiplies in the haemolymph. When a louse is crushed, the infected haemolymph is released onto the human skin from where the pathogen enters the body through abrasions, wounds or mucous membranes [22]. In 2015, 27 confirmed cases of louse-borne relapsing fever were reported among refugees from countries in the Horn of Africa [24].
Other louse-borne infections
Head lice can transmit two opportunistic bacteria, Staphylococcus aureus and Streptococcus pyogenes on their external surfaces, mechanically [25]. Other pathogens have also been identified in head lice (Coxiella burnetii, Rickettsia aeschlimannii, Acinetobacter baumannii) but the role of head lice in their transmission is unknown [5]. Yersinia pestis was isolated from a body louse collected from a patient during a plague outbreak in Morocco [26] and it has been experimentally shown that body lice can transmit the pathogen [11].
In animals, chewing lice do not have an important vectorial role. However, some species (i.e. the lice of carnivores) are intermediate hosts for Dipylidium caninum which is transmitted to dogs and cats via ingestion. Some lice infesting birds are able to transmit avian filariases [2,3]. Sucking lice infesting animals can transmit certain pathogens, such as swine pox virus and bovine anaplasmosis [27].
Public health control measures
In the case of humans, the management of lice requires differing treatment methods, depending on the species. Delousing is considered the best way to control louse-borne diseases [4]. To control the body lice infestation, regular showering or bathing together with regular washing and changing of clothes and linen/blankets is essential [5], particularly in crowded places such as refugee camps, shelters for the homeless and prisons. Several case studies have demonstrated the effectiveness of these methods [28] [29]. In addition to controlling the louse infestation, confirmed cases of body louse-borne infections should be immediately treated using antibiotics [5]. To control head lice, mechanical removal of lice and nits is necessary, combined with treatment of the scalp using various pediculicides. As products are generally only effective against adults and nymphs, treatment should be repeated after 10−14 days [5]. Although certain products claim to have an ovicidal activity, this is generally limited, and a second treatment is recommended for all products, except for the topical 0.5% ivermectin [30].
Scalp shaving is also an efficient method of control [22] and pubic lice can also be controlled by combing or shaving the pubic hair. An effective way to remove lice from clothes and linen is to heat them (i.e. air-drying) to 60°C or wash them for 30 minutes at 55°C, or for a shorter period at a higher temperature [31].
In cattle, effective treatments against chewing lice include dipping or spraying with pyrethroids or formamidines. All these are effective against nymphs and adults but cannot kill the eggs. As the residual effect does not last long, the treatment should be repeated after 14−20 days. Pour-on products are also available with similar insecticides as the products above. These can also be used in combination (i.e. organophosphates + pyrethroids) or pour-on products with macrocyclic lactones (ivermectin, moxidectin, eprinomectin). Injectable macrocyclic lactones are not effective against chewing lice. In sheep, the preventive autumn dipping against psoroptic mange is also effective against lice. In dogs and cats, as there are no repellent products against lice, the preferred approach is to treat infected animals. Various pharmaceutical treatments are available: topical application treatments (fipronil, cyphenothrin, imidacloprid, permethrin, moxidectin, selamectin, metaflumizone), collars (e.g. flumethrin plus imidacloprid ). Note that permethrin is toxic for cats. For the control of sucking lice infesting animals, the same approaches apply as for chewing lice. In addition, injectable macrocyclic lactones are available but this treatment must be repeated after two-to-three weeks.
Key areas of uncertainty
Louse-borne diseases are relatively neglected in Europe compared to other vector-borne diseases in terms of targeted surveillance, research and control. One of the main knowledge gaps in understanding the risks of pathogen transmission from lice to humans is the lack of studies on the prevalence of body-lice in risk groups across most of the EU and the lack of surveillance of louse-borne pathogens. Other gaps relate to our understanding of the vectorial role of head lice, as for several pathogens detected in lice, the transmission potential has not been demonstrated [15].
References
1. Lehane MJ. The biology of blood-sucking in insects. Second edition. Cambridge: Cambridge University Press; 2005 (321).
2. Deplazes P, Eckert J, Mathis A, Von Samson-Himmelstjerna G, Zahner H. Parasitology in veterinary medicine. First edition. Wageningen: Wageningen Academic Publishers; 2016 (653).
3. Durden LA. Lice (Phthiraptera). In: Mullen GR, Durden LA, editors. Medical and Veterinary Entomology. London: Academic Press; 2002 (171-90).
4. Badiaga S, Brouqui P. Human louse-transmitted infectious diseases. Clinical Microbiology and Infection. 2012 Apr;18(4):332-7.
5. Coates SJ, Thomas C, Chosidow O, Engelman D, Chang AY. Ectoparasites: pediculosis and tungiasis. Journal of the American Academy of Dermatology. 2020 Mar;82(3):551-69.
6. Badiaga S, Menard A, Tissot Dupont H, Ravaux I, Chouquet D, Graveriau C, et al. Prevalence of skin infections in sheltered homeless. European Journal of Dermatology. 2005 Sep-Oct;15(5):382-6.
7. Li W, Ortiz G, Fournier PE, Gimenez G, Reed DL, Pittendrigh B, et al. Genotyping of human lice suggests multiple emergencies of body lice from local head louse populations. PLoS Neglected Tropical Diseases. 2010 Mar 23;4(3):e641.
8. Angelakis E, Bechah Y, Raoult D. The history of epidemic typhus. Microbiology Spectrum. 2016 Aug;4(4).
9. Bauer E, Jahnke C, Feldmeier H. Seasonal fluctuations of head lice infestation in Germany. Parasitology Research. 2009 Feb;104(3):677-81.
10. Bechah Y, Capo C, Mege JL, Raoult D. Epidemic typhus. Lancet Infectious Diseases. 2008 Jul;8(7):417-26.
11. Houhamdi L, Lepidi H, Drancourt M, Raoult D. Experimental model to evaluate the human body louse as a vector of plague. Journal of Infectious Diseases. 2006 Dec 1;194(11):1589-96.
12. Akram SM, Ladd M, King KC. Rickettsia prowazekii. [Updated 20 September 2021] StatPearls. Treasure Island (FL): StatPearls Publishing; Jan 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448173/
13. Portillo A, Santibanez S, Garcia-Alvarez L, Palomar AM, Oteo JA. Rickettsioses in Europe. Microbes and Infection 2015 Nov-Dec;17(11-12):834-8.
14. Niang M, Brouqui P, Raoult D. Epidemic typhus imported from Algeria. Emerging Infectious Diseases. 1999 Sep-Oct;5(5):716-8.
15. Zanetti G, Francioli P, Tagan D, Paddock CD, Zaki SR. Imported epidemic typhus. Lancet. 1998 Nov 21;352(9141):1709.
16. Faucher JF, Socolovschi C, Aubry C, Chirouze C, Hustache-Mathieu L, Raoult D, et al. Brill-Zinsser disease in Moroccan man, France, 2011. Emerging Infectious Diseases. 2012 Jan;18(1):171-2.
17. Ericsson CD, Jensenius M, Fournier PE, Raoult D. Rickettsioses and the international traveler. Clinical Infectious Diseases. 2004 Nov 15;39(10):1493-9.
18. Okorji O, Olarewaju O, Pace WC. Trench fever [Updated 12 Feb 2021]. StatPearls. Treasure Island (FL) 2021. StatPearls Publishing; Jan 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562259/
19. Guibal F, de La Salmoniere P, Rybojad M, Hadjrabia S, Dehen L, Arlet G. High seroprevalence to Bartonella quintana in homeless patients with cutaneous parasitic infestations in downtown Paris. Journal of the American Academy of Dermatology. 2001 Feb;44(2):219-23.
20. Brouqui P, Houpikian P, Dupont HT, Toubiana P, Obadia Y, Lafay V, et al. Survey of the seroprevalence of Bartonella quintana in homeless people. Clinical Infectious Diseases. 1996 Oct;23(4):756-9.
21. Angelakis E, Rolain JM, Raoult D, Brouqui P. Bartonella quintana in head louse nits. FEMS Immunology and Medical Microbiology. 2011 Jul;62(2):244-6.
22. Warrell DA. Louse-borne relapsing fever (Borrelia recurrentis infection). Epidemiology and Infection. 2019 Jan;147:e106.
23. Amanzougaghene N, Akiana J, Mongo Ndombe G, Davoust B, Nsana NS, Parra HJ, et al. Head lice of Pygmies reveal the presence of relapsing fever borreliae in the Republic of Congo. PLoS Neglected Tropical Diseases. 2016 Dec;10(12):e0005142.
24. European Centre for Disease Prevention and Control (ECDC). Rapid risk assessment. Louse-borne relapsing fever in the EU. 17 November 2015. Stockholm: ECDC; 2015.
25. Burkhart CN, Burkhart CG. Fomite transmission in head lice. Journal of the American Academy of Dermatology. 2007 Jun;56(6):1044-7.
26. Drancourt M, Houhamdi L, Raoult D. Yersinia pestis as a telluric, human ectoparasite-borne organism. Lancet Infectious Diseases. 2006 Apr;6(4):234-41.
27. Russell RC, Otranto D, Wall RL. The Encyclopedia of Medical and Veterinary Entomology: CABI; 2013.
28. Raoult D, Ndihokubwayo JB, Tissot-Dupont H, Roux V, Faugere B, Abegbinni R, et al. Outbreak of epidemic typhus associated with trench fever in Burundi. Lancet. 1998 Aug 1;352(9125):353-8.
29. Sundnes KO, Haimanot AT. Epidemic of louse-borne relapsing fever in Ethiopia. Lancet. 1993 Nov 13;342(8881):1213-5.
30. Bowles VM, Hanegraaf S, Ahveninen T, Sidgiddi S, Allenby K, Alsop H. Effect of a new head lice treatment, Abametapir lotion, 0.74%, on louse eggs: a randomized, double-blind study. Global Pediatric Health. 2019;6:2333794X19831295.
31. Bacot AW. The Louse problem. Proceedings of the Royal Society of Medicine.1917;10:61–94.