Overall situation
Disease background
Viral hepatitis is an infection that causes inflammation of the liver. It can be caused by different viruses, including hepatitis B virus (HBV) and hepatitis C virus (HCV). Both HBV and HCV can cause acute and chronic infections and are leading causes of liver cirrhosis and hepatocellular carcinoma.
Worldwide, the latest estimates indicate that around 296 million people are living with a chronic HBV infection and 58 million people are living with a chronic HCV infection [2].
In the EU and EEA, there has been a decline in the reported number of new transmissions of HBV and HCV, resulting in a reduction in incidence [3, 4]. However, based on an analysis of prevalence estimates published up to 2015, it was estimated that in the EU/EEA there remain approximately 3.6 million people living with chronic HBV infection [5]. Based on recent modelling work to produce national estimates of HCV RNA prevalence it is estimated that there are 2.4 million individuals with chronic HCV [6].
Despite a reduction in the incidence of HBV and HCV, viral hepatitis remains a leading cause of hepatitis-related mortality.
Globally, HBV and HCV cause 1.1 million deaths per year [2]. Based on data from 2015, it is estimated that across the EU/EEA and the United Kingdom, HBV and HCV are responsible for approximately 55% of all liver cancer deaths and 45% of all deaths due to cirrhosis and other chronic liver disease and result in approximately 64 000 deaths annually [7].
Prevalence of hepatitis B and C
Prevalence
ECDC has collected estimates of hepatitis B surface antigen (HBsAg) in the general population from EU/EEA countries. HBsAg prevalence estimates are available from 16 countries, with estimates ranging from 0.1% in Ireland to 4.5% in Romania (Figure 1) [8].
For hepatitis C, available data on prevalence are also incomplete, and many countries lack up to date and robust prevalence estimates. ECDC is working with countries to support the undertaking of standardised epidemiological studies and to develop national estimates of burden through modelling approaches. National estimates of HCV RNA prevalence have been recently produced based on prevalence estimates in the general population and among people who inject drugs (PWID) using a multi-parameter evidence synthesis method [6]. The preliminary results indicate that national estimates of RNA prevalence range from ≤0.1 in the Netherlands, Slovenia, and Iceland to 2.3% in Romania (Figure 1).
Estimates of hepatitis B surface antigen (HBsAg) prevalence in the general population based on pooled estimates of prevalence up to 2021
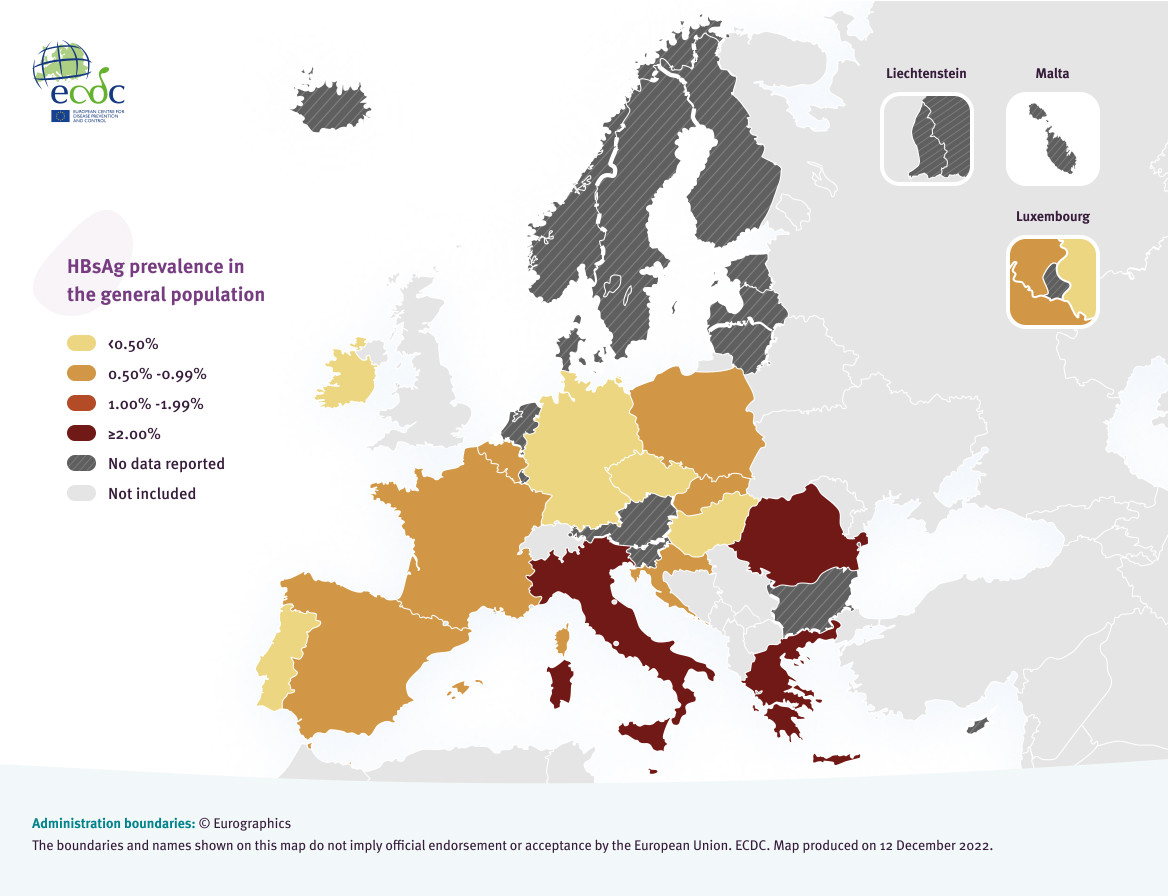
1a. Estimates of hepatitis B surface antigen (HBsAg) prevalence in the general population based on pooled estimates of prevalence up to 2021 | Source: [8]
National estimates of hepatitis C RNA prevalence, 2022
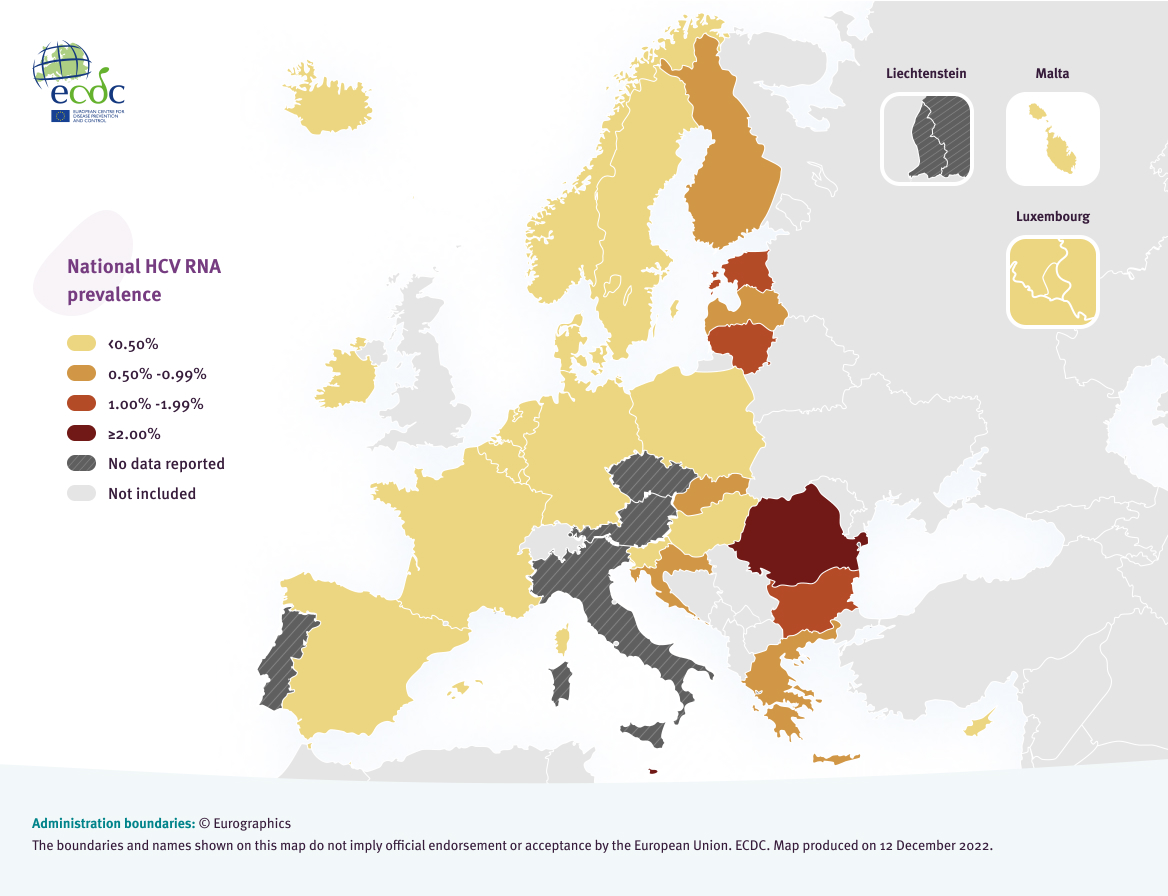
Source: [6]
Route of transmission
HBV and HCV are blood-borne infections, have multiple routes of transmission and affect a variety of key populations, leading to a complex prevention landscape. Figure 2 identifies the reported route of transmission for acute hepatitis B and C infections in EU/EEA countries in 2020 reported to ECDC. Acute infections reflect new transmissions in the EU/EEA and the prevention of these transmissions are a key target for prevention measures.
HBV
Data on likely route of transmission of HBV were only available for 29% of acute cases reported in 2020, representing 19 countries [4]. The incompleteness of the data is a major challenge for the interpretation of the results. Available data show that heterosexual transmission (32%), sex between men (14%), and transmission in healthcare settings (nosocomial transmission) (12%) account for over half of acute HBV case transmissions (Figure 2). Six countries reported acute cases attributable to nosocomial transmission and of these, two countries, Italy and Poland, accounted for 77%, indicating marked variation between countries. The reported route of transmission for acute cases, which represents current transmission, indicates that only 1% of cases with available data were attributed to mother to child transmission suggesting that vertical transmission of HBV is uncommon across EU/EEA countries, but strategies to prevent transmission via this route are still vital because the majority of newborns infected perinatally will develop chronic infection. The most common transmission route for chronic HBV cases was vertical transmission, accounting for 52% of cases with a reported transmission route, but it should be noted that the majority (77%) of these cases were classified as imported cases from outside the reporting country.
HCV
Data on likely route of transmission of HCV were only available for 31% of cases reported in 2020, representing 13 countries, again making interpretation difficult [9]. The most common routes of transmission for acute HCV cases were injecting drug use (55%), and sex between men (18%) (Figure 2). Sixty-nine percent of chronic HCV cases were attributed to injecting drug use. With low rates of data on route of transmission and substantial variation between countries, data are not likely to be fully representative. In addition, it should be noted that the data on transmission may be subject to a diagnostic bias among groups who may more likely than others to be tested sequentially and in whom the infection, which is frequently asymptomatic, is thus more likely to be identified.
However, in spite of the challenges around the data, it is clear that PWID are a key risk group in the region.
Transmission category of acute hepatitis B and C cases in the EU/EEA, 2020 [1]

Source: ECDC. Hepatitis B: Annual Epidemiological Report for 2020 [4]; ECDC. Hepatitis C: Annual Epidemiological Report for 2020 [9]
Some population groups can have overlapping, multiple risk factors for hepatitis acquisition, including men who have sex with men (MSM), PWID, people in prison and people migrating from intermediate/high endemic areas [10]. Robust data on sizes of key populations and prevalence in key populations are often lacking, but estimates are available for some European countries. PWID are the population group with the highest prevalence of antiHCV infection in the EU/EEA, with prevalence estimates ranging from 15.4% to 70.5% [6]. HBV infection is also prevalent in this population, with estimates ranging from 0% to 16.9% [8]. People in prisons and some migrant populations have the highest prevalence of HBV in the EU/EEA, with prevalence estimates ranging from 0.3% to 24.9% for people in prison and from 0.1% to 31.7% for migrant populations [8].
[1] Cases with known transmission status