Epidemiological update of 29 April on avian influenza A(H7N9) virus
Since 31 March 2013, one hundred and twenty one (121) cases of human infection with avian influenza A(H7N9) virus have been reported from eight provinces and two municipalities in eastern China and one (1) from Taiwan.
Since 31 March 2013, one hundred and twenty one (121) cases of human infection with avian influenza A(H7N9) virus have been reported from eight provinces and two municipalities in eastern China and one (1) from Taiwan. Onset of disease has been between 19 February and 19 April 2013 in: Anhui (4), Fujian (1), Henan (4), Hunan (1), Jiangsu (26), Jiangxi (3), Shandong (1) and Zhejiang (45) and two Municipalities: Beijing (1) and Shanghai (34), and one case with no fatalities reported from the Taiwan (1) on 24 April 2013. The date of disease onset is currently unknown for thirteen patients.
The health authorities in the areas affected are responding to this public health event by enhanced surveillance, epidemiological and laboratory investigation and contact tracing. The animal health sector has intensified investigations into the possible sources and reservoirs of the virus. The Chinese authorities reported to the World Organisation for Animal Health (OIE) that avian influenza A(H7N9) was detected in samples from pigeons, chickens and ducks, and in environmental samples from live bird markets ('wet markets') in Shanghai, Jiangsu, Anhui and Zhejiang provinces. Authorities have closed markets and culled poultry in affected areas.
The source and mode of transmission have not been confirmed. The outbreak is caused by a reassortant avian influenza virus with low pathogenicity for birds, hence it does not cause the signal 'die-offs' in poultry associated with highly pathogenic strains of avian influenza viruses. Genetic analyses of the isolates have shown changes which suggest that the H7N9 virus may have greater ability to infect mammalian species, including humans, than most other avian influenza viruses. Pathogenicity for humans appears to be high and higher age appears to be a risk factor for disease.
The most likely scenario is that the influenza A(H7N9) virus is spreading undetected in poultry populations and occasionally infecting humans who have close contact with poultry or poultry products but this will have to be validated as further data become available.
At the present time there is no evidence of sustained human-to-human transmission. Close to 2 000 close contacts of confirmed cases are reported to have been followed up. There is one family cluster with two confirmed cases for which human-to-human transmission cannot be ruled out but where common exposure is the most likely explanation. In addition, the virus has been detected in one asymptomatic carrier in Beijing.
An increasing incidence of sporadic cases and expansion of geographic spread in China and possibly neighbouring countries are expected over the coming weeks. Individual imported human cases to Europe cannot be ruled out and countries need to prepare for detecting and diagnosing such cases.
Critical developments that would change this assessment would be evidence of sustained human-to-human transmission and detection of avian influenza A(H7N9) in bird populations in Europe.
ECDC has published the Supporting diagnostic preparedness for detection of avian influenza A(H7N9) viruses in Europe guidance for laboratories on 24 April 2013.
ECDC is preparing an EU case definition for A(H7N9).
ECDC is closely monitoring developments and is continuously re-assessing the situation in collaboration with WHO, US CDC, China CDC and other partners.
This epidemiological update does not change the conclusions and recommendations of the updated risk assessment published on April 12.
Figure 1. Distribution of influenza A(H7N9) cases by week of onset of symptoms, as of 29 April 2013 (n=121, no onset dates for 13 cases, missing 5 fatalities) (the latest disease onset reported 19 April 2013 in week 16)
Figure 2. Distribution of influenza A(H7N9) cases by week of reporting, as of 29 April 2013 (cases (incl. fatalities)=121, fatalities=23, CFR=19%)
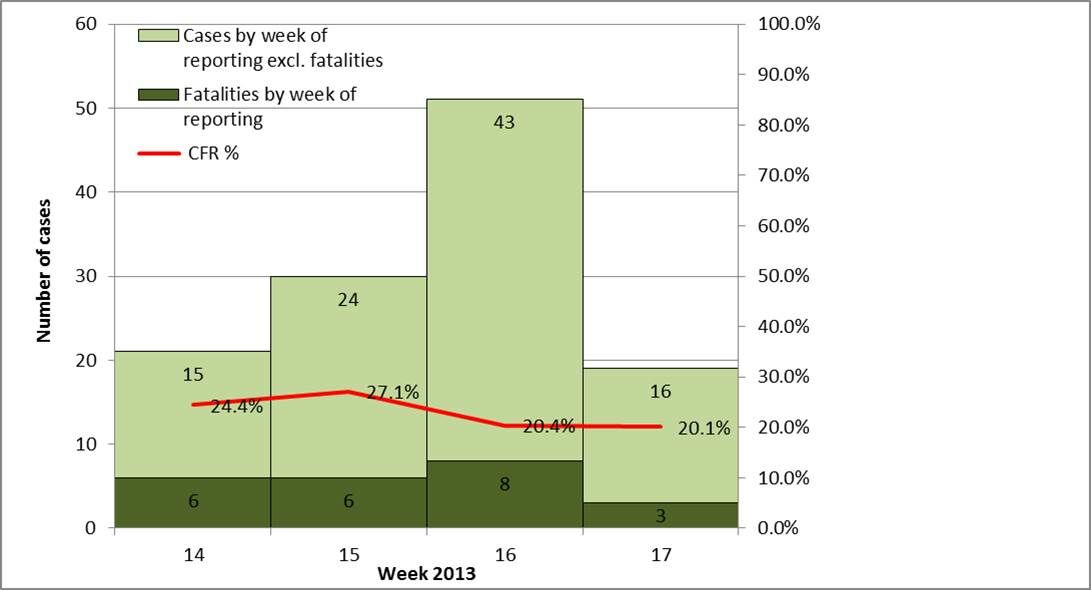
Figure 3. Distribution of influenza A(H7N9) cases, by place of reporting, as of 29 April 2013
Figure 4. Distribution of cumulative number of influenza A(H7N9) cases, 19 February-29 April 2013






