Key interventions to prevent and control infections among people who inject drugs
Six interventions, one aim: to prevent and control infections among people who inject drugs. In new public health guidance released today, the European Centre for Disease Prevention and Control (ECDC) and the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) have joined forces to identify key interventions to address infectious diseases in this population. Reflecting on new evidence, infectious disease treatments, and public health concepts, this guidance updates the 2011 edition.
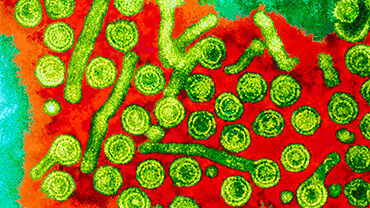
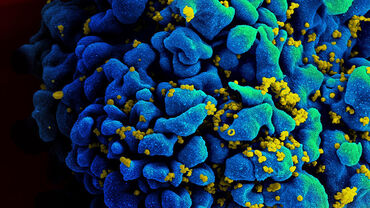
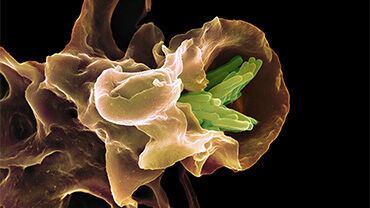
Injecting drug use remains a crucial risk factor for acquiring blood-borne viruses such as hepatitis B and C, and HIV, but also other infectious diseases, such as sexually transmitted infections (STIs) and tuberculosis (TB). While for STIs and TB, injecting drugs does not directly cause infection, factors such as living conditions or higher-risk sexual practices place some people who inject drugs at a greater risk.
Several of the diseases covered by the guidance are the focus of the United Nations Sustainable Development Goal (SDG) Target 3.3, where countries have committed to end AIDS and tuberculosis and combat hepatitis by 2030. Achieving the SDG target will not be possible unless these diseases are tackled in all populations, including people who inject drugs.
ECDC Director Andrea Ammon said:
“There are better and more effective tools than ever before to prevent, detect and treat infections associated with injecting drug use. However, access to these services is often hindered by barriers like stigma, discrimination, or legal concerns. When designing strategies, policies, and programmes to address infectious diseases among people who inject drugs, policy-makers and public health planners should consider approaches that limit and overcome these barriers and that promote service accessibility, uptake and coverage through the combined provision of interventions”.
EMCDDA Director Alexis Goosdeel said:
“Changes in the European drug market and in drug use patterns in recent years have created new challenges. Stimulant injecting, often in combination with opioids, for example, has resulted in infectious disease outbreaks in several EU cities. This updated guidance reiterates the need for countries to expand their coverage of a number of life-saving harm-reduction and treatment services which have proven to be effective in preventing and controlling infectious diseases among people who inject drugs. We have the knowledge. We now need to ensure that these interventions are delivered at optimal scale.”
Over the last decade, there has been a steady reduction in the number of HIV diagnoses among people who inject drugs. However, since 2015, very few EU/EEA countries have seen a substantial decrease in the transmission of hepatitis C virus (HCV) among people who inject drugs. Notably, hepatitis C tends to be more common than HIV among people who inject drugs, and a history of injecting drug use is the most frequently reported risk factor in EU/EEA countries for acquiring this.
Ultimately, infections associated with the sharing of contaminated injecting equipment or with other modes of transmission impact individuals' quality of life and life expectancy.
They can also lead to both direct and indirect societal costs through, for example, lost productivity, high treatment and care costs, and risk of onward transmission of infectious diseases to others, including those who do not inject drugs.
This joint guidance reinforces the need for a comprehensive and coordinated approach to addressing the persistent public health challenge of drug-related infections in EU/EEA countries. Ultimately, it aims to improve the well-being and health outcomes of individuals affected by these issues.
The six key intervention areas and recommendations proposed in the guidance range from the provision of sterile injection equipment, testing, and vaccination, to the treatment of infections and drug dependence. They are:
-
Sterile injection equipment – provide sterile needles and syringes and other drug preparation equipment (cookers, filters and water for injection), including in prisons and through pharmacies.
-
Drug dependence treatment – provide opioid agonist treatment (OAT), including in prisons, for people who are dependent on opioids. OAT should be offered in conjunction with sterile injecting equipment and information, education, and counselling.
-
Vaccination – offer vaccinations against hepatitis A and B, respiratory infections and tetanus, as well as the pneumococcal and the human papillomavirus vaccines for people living with HIV who inject drugs.
-
Testing – routinely offer voluntary and confidential infectious disease testing and link all people with a positive test result to care.
-
Infectious disease treatment – offer infectious disease treatment according to national and international guidelines, ensure there is good cooperation and links between service providers dedicated to people who inject drugs and infectious disease care; involve peer mentors to strengthen adherence to treatment.
-
Drug consumption rooms – provide supervised injecting facilities to reduce injecting risk behaviour among people who inject drugs, which could as a consequence contribute to the prevention of HCV and HIV transmission.
For the maximum effectiveness of interventions, coordination between health, drug, and social services sectors is essential. Additionally, these interventions should be delivered in combination with each other and with health promotion activities that target structural and individual factors that promote healthier and/or safer behaviours.
With this guidance, ECDC and the EMCDDA aim to support policy-makers, drug professionals, and civil society organisations by providing an evidence base to inform national strategies, policies, and programmes for people who inject drugs.