Epidemiological update: Middle East respiratory syndrome coronavirus (MERS-CoV), 21 July 2015
Since the previous update of the ECDC Rapid Risk Assessment on MERS-CoV (30 June 2015), 13 new cases and seven deaths have been reported globally from South Korea (4 cases and 4 deaths), Saudi Arabia (8 cases and 3 deaths) and the Philippines who reported a travel-related MERS case related to travel in the Middle East on 6 July 2015.
Since April 2012 and as of 21 July 2015, 1 392 cases of MERS (including 538 deaths) have been reported by health authorities worldwide (Figure 1 and Table 1).
Figure 1. Distribution of confirmed cases of MERS by month* and probable place of acquisition of infection, March 2012–21 July 2015 (n=1 392)

Since the previous update of the ECDC Rapid Risk Assessment on MERS-CoV (30 June 2015), 13 new cases and seven deaths have been reported globally from South Korea (4 cases and 4 deaths), Saudi Arabia (8 cases and 3 deaths) and the Philippines who reported a travel-related MERS case related to travel in the Middle East on 6 July 2015.
The majority of cases have occurred in the Middle East, most of them in Saudi Arabia and the United Arab Emirates (Table 1). However, South Korea has reported the highest number of new cases since the start of the outbreak there in early May 2015.
Table 1. Confirmed MERS cases and deaths, by country of reporting, March 2012–21 July 2015
| Reporting country | Cases | Deaths |
|---|---|---|
| Middle East | 1 179 | 491 |
| Saudi Arabia | 1 048 | 462 |
| United Arab Emirates | 81 | 11 |
| Jordan | 19 | 6 |
| Qatar | 13 | 5 |
| Oman | 6 | 3 |
| Iran | 6 | 2 |
| Kuwait | 3 | 1 |
| Egypt | 1 | 0 |
| Yemen | 1 | 1 |
| Lebanon | 1 | 0 |
| Europe | 15 | 8 |
| United Kingdom | 4 | 3 |
| Germany | 3 | 2 |
| France | 2 | 1 |
| Netherlands | 2 | 0 |
| Greece | 1 | 1 |
| Turkey | 1 | 1 |
| Austria | 1 | 0 |
| Italy | 1 | 0 |
| Asia | 191 | 37 |
| China | 1 | 0 |
| Malaysia | 1 | 1 |
| Philippines | 3 | 0 |
| South Korea | 185 | 36 |
| Thailand | 1 | 0 |
| Rest of the world | 7 | 2 |
| Algeria | 2 | 1 |
| Tunisia | 3 | 1 |
| United States of America | 2 | 0 |
| Total | 1 392 | 538 |
All cases reported from outside the Middle East have either had a recent travel history to the Middle East or could be linked to a chain of transmission originating from a case with a travel history to the Middle East (Figure 2).
Figure 2. Distribution of confirmed MERS cases by probable place of acquisition of infection, as of 21 July 2015 (n=1 392)

South Korea
On 20 May 2015, the Korea Centres for Disease Control and Prevention notified WHO of the first laboratory-confirmed case of MERS in a 68-year-old man with recent travel history to the Middle East.
As of 21 July 2015, the South Korean Ministry of Health and Welfare reported 186 cases since the beginning of the outbreak in South Korea (including the index case and the South Korean case reported by China). Of these, 136 patients have been discharged, 36 patients have died and 14 are still receiving medical treatment. Twelve of the 14 cases under treatment have twice tested negatively for MERS-CoV and nine of them are receiving care in general wards.
The last case from South Korea was reported on 4 July 2015. Transmission can be considered to have ended when no new cases are detected for a period of 28 days (two times the maximum 14 day incubation period) after the last case being treated has tested negative two times (with a minimum of 24 hours between the two tests) or the case has died.
Figure 3. Distribution of confirmed cases of MERS by date of onset or reporting, South Korea and China, 11 May–21 July 2015 (n=186)
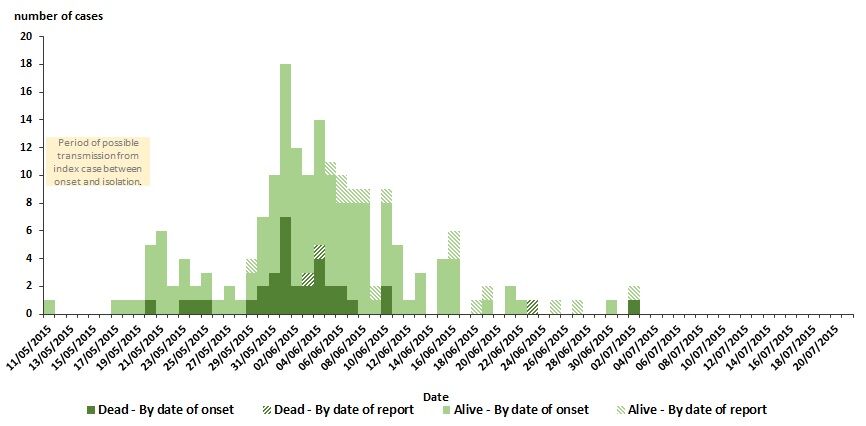
The index case in the South Korean outbreak had onset of symptoms on 11 May and was diagnosed and isolated on 20 May 2015. During the 10-day period from onset of illness until isolation (Figure 3, yellow box), the index case visited several healthcare facilities. According to local health authorities, The Samsung medical hospital was released from quarantine on 20 July 2015 as all the conditions for infection control had been met. This was the last hospital out of 15 affected hospitals freed from quarantine.
All reported cases apart from two (the index case and the suspected household transmission) have been associated with nosocomial transmission in South Korea. As of 28 June 2015, the South Korean Ministry of Health reported that 39 of 186 (21%) of the cases are healthcare workers: 23 doctors or nurses, eight caregivers, two radiographers, two ambulance workers, one computing personnel, one transfer staff and two security guards.
ChinaOn 30 May 2015, WHO reported a case of MERS in China with probable transmission in South Korea. The case is the son of the third MERS case in South Korea and the younger brother of the fourth MERS case. He visited his father at a time when he was hospitalised in the same room as the index case in South Korea. Later, he travelled from Seoul to Guangdong in China where he was hospitalised, and MERS-CoV infection was confirmed on 29 May. No further cases of MERS linked to this patient have been identified to date. According to media sources, the patient was discharged from hospital on 26 June 2015.
The PhilippinesOn 6 July 2015, The Philippines Department of Health reported that a non-national male, who developed symptoms of MERS on 30 June 2015, had a laboratory-confirmed positive result for MERS-CoV on 4 July 2015. The case was discharged following two negative tests, 48 hours apart on 10 July 2015.
According to public health authorities in the Philippines, as a precautionary measure, 36 close contacts will remain under observation for 14 days after their last contact with the case, and further contact tracing is ongoing.
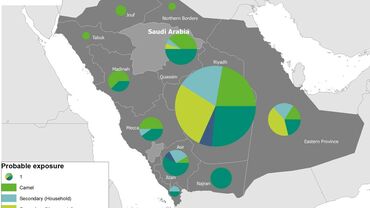
Saudi ArabiaSince the beginning of 2015 and as of 21 July, Saudi Arabia has reported 222 infections with MERS-CoV (Figure 4).
Figure 4. Distribution of MERS cases by reporting city, Saudi Arabia, 1 January–21 July 2015

Travel advice Countries should advise travellers returning from all countries affected by MERS to seek medical attention if they develop a respiratory illness with fever and cough during the two weeks after their return and to disclose their recent travel history to the healthcare provider. The travellers, especially with pre-existing medical conditions, should be reminded of the importance of good hand and food hygiene, and to avoid contact with sick people. In addition, travellers to the Arabian Peninsula should avoid close contact with camels, visiting farms and consuming unpasteurised camel milk, urine or improperly cooked meat.
This year the Hajj falls between 21 and 26 September. Hajj and Umrah travellers with pre-existing medical conditions should be advised to consult a healthcare provider to review the risk before deciding to make the pilgrimage.
Travellers with pre-existing medical conditions should be advised to identify a trusted healthcare facility prior to travel in case of a health emergency during their stay. Travellers who require medical care should minimise contact with other sick people in the facility.