Weekly epidemiological update: Omicron variant of concern (VOC) – week 1 (data as of 7 January 2022) EU/EEA
Over the past two weeks, a steep increase in COVID-19 notification rates has been observed in several EU/EEA countries.
For a general overview of the epidemiological COVID-19 situation in the EU/EEA, please see the weekly ECDC Country Overview Report. At the end of week 52, high and increasing case notification rates or an epidemiological situation of high or very high concern were observed in all but two EU/EEA Member States. This situation is largely driven by the continued circulation of the Delta variant and rapidly increasing spread of the Omicron variant in many countries.
The summary below aims to give an overview of the extent to which Omicron is prevalent in EU/EEA countries. The data are collected from The European Surveillance System (TESSy), EU/EEA Member States’ national and/or regional websites, and media reports quoting health authorities. As a result, the data presentation and completeness might be different depending on the data sources and availability on countries’ websites.
In EU/EEA countries that use faster methods to screen for the Omicron VOC (variant-specific PCR tests and/or S gene target failure rather than full sequencing) and publish these data, the estimated prevalence of the Omicron VOC for the most recent date available was:
• Denmark: 92.5% (2 January 2022)
• France: 80.3%% (2021-w52)
• Iceland: 70% from one laboratory (21 December 2021)
• Ireland: 96% (5 January 2022)
• Italy: 28% (23 December 2021)
• Luxembourg: 32.4% (2021-w51)
• Netherlands: 76.9% ranges between labs 76.3%-90.8% (2 January 2022)
• Portugal: 75% (27 December 2021)
• Romania: 17.7% (2021-w52)
Several additional countries publish full sequencing results or do not specify the type of method used. Please note that, due to the lag between sampling and sequencing, for some countries these results may show the situation with several weeks’ lag:
• Austria: 61% (2021-w52)
• Belgium: 97.8% (2021-w52)
• Bulgaria: 4.4% (samples taken between 15 November and 22 December)
• Czechia: 46.7% (2021-w52)**
• Cyprus: 50% (2021-w51)**
• Estonia: 55% (29 December 2021)*
• Finland: 36.1% (2021-w51)** And 90% in Helsinki (5 January 2022)*
• Germany: 20% (2021-w51) **
• Greece: 40% (2021-w52)** And +/- 70% in five regions of Greece (3 January 2022)
• Hungary: over 11% (as of 5 January 2022) *
• Latvia: 16.9% (2021-w52)
• Lithuania: 32% (2021-w51)**
• Malta: 89.5% (2021-w51) **
• Norway: 67.7% (3 January 2022)
• Poland: 11.3% (2021-w52)**
• Slovakia: 3.9% (2021-w52)**
• Slovenia: estimated 40% (samples from 31 December 2021)*
• Spain: 68.2% (2021-w51)**
• Sweden: 91.7% (2021-w52)**
* Type of test not specified
** Insufficient precision at less than 5% prevalence
Countries for which no national proportion was available:
• Croatia: 8 cases (15 December 2021)
• Liechtenstein: 15 cases using targeted sequencing (as of 5 January 2022). Switzerland and Liechtenstein together have 64.20% Omicron on a seven-day average and 83.90% as a daily value on 19 December 2021 using full and targeted sequencing of a representative sample.
The ECDC dashboard on Variants of Concern (beta version) shows the evolution over time, including for the Omicron VOC.
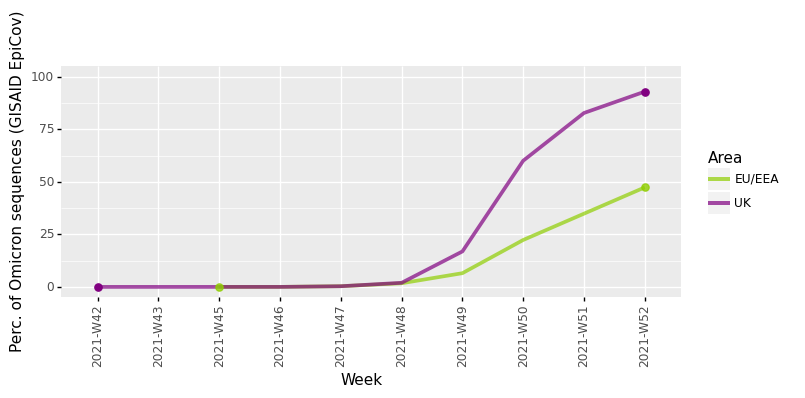
Data from GISAID show the evolution of the proportion of samples uploaded that are due to the Omicron variant over recent weeks. Although these data may be affected by reporting lags and could be revised in coming weeks as additional data are reported, it is evident that the prevalence of Omicron in the EU/EEA is increasing (Figure 1).
Figure 1. Percentage of SARS-CoV-2 sequences in GISAID EpiCov that are due to the Omicron VOC as of 4 January 2022
Disease severity related to Omicron
The current limited and preliminary evidence suggests that Omicron has a less severe clinical presentation. However, it is still premature to make a complete assessment of Omicron’s severity, and more research and data, including from the EU/EEA countries, are required in order to fully determine the effect and to assess if it applies to all population groups, considering differences in vaccination coverage and population composition.
Recently published but not peer-reviewed data from Gauteng Province in South Africa show that despite recording a higher number of SARS-CoV-2 cases during the Omicron wave, hospital admission rates were lower (4.9%) than in the previous waves (Beta 18.9%, Delta 13.7%). Likewise, fewer patients had severe disease during the Omicron wave (28.8%) than the Beta (60.1%) and Delta (66.8%) waves. The median length of hospital stay was with 4 days (IQR 2-6) also shorter in the most recent wave than in the Beta and Delta waves (7 days (IQR 4-11) and 8 days (IQR 4-14), respectively). Omicron hospitalised patients were 73% less likely to be severely ill than patients admitted during the preceding waves (aOR 0.27, 95% CI 0.25-0.31). However, it is important to consider that 73% of the adult population in Gauteng Province was already infected before the Omicron dominance.
The UK Health Security Agency shared a report estimating that Omicron infected individuals have 50% lower risk to visit or to be admitted to the hospital than people with infection due to Delta variant (hazard ratio 0.53, 95% CI 0.50-0.57). They also found a 65% lower hospitalisation risk for Omicron cases who had received 2 doses of a vaccine and 81% reduction with 3 doses, compared to unvaccinated Omicron cases.
Another study from Scotland used the national data of individuals with symptomatic Omicron infection and identified a reduced hospitalisation risk compared to Delta cases, while the rate of possible reinfection for Omicron was 10 times that of Delta. Vaccinated individuals with the third/booster dose had a 57% (95% CI 55-60) lower risk to experience symptoms following Omicron infection.
A recent Canadian report confirmed low hospital admission rates (0.3%) and case fatality (<0.1%) for Omicron cases. Shorter median length of hospital stay and reduced need for respiratory support than the previous variants were also reported in another publication (not peer-review) from Texas.
It usually takes several weeks for the accumulation of clinical outcomes to conclude on the impact of a specific variant in hospital admissions, intensive care need and deaths. It is important to highlight that prior immunity from natural infection and/or vaccination and improved treatment options will contribute to less severe outcomes from subsequent infection. The true risk of severe infection may be underestimated by the large numbers of vaccinated or previously infected people, which was not the case in the beginning of preceding waves. It is also essential to account for the relatively young age of most people who have been infected with Omicron so far, and thus far there is little data on the severity among older age-groups and people with underlying risk factors.
Therefore, early results may not represent the entire Omicron wave and the clinical profile of Omicron may change with upcoming evidence. Importantly, the combination of higher growth rate and immune evasion indicate that any potential advantage Omicron may have in terms of decreased severity, could be countered by increased community infection rates leading to substantially additional burden for the hospitals, while primary care may be overburdened even more than during previous waves. As more evidence accumulates, a better assessment of clinical outcomes and long-term consequences, such as post-COVID-19 condition will be feasible.
Vaccine effectiveness against infection and/or severe disease due to Omicron
Preliminary data from UK and Denmark show a significantly reduced vaccine effectiveness against symptomatic disease with Omicron VOC compared to Delta VOC, which further rapidly declines few months after dose 2, and by 10 weeks after dose 3. This waning is faster with the Omicron VOC than with the Delta VOC. A booster dose confers a stronger protection against symptomatic disease due to the Omicron VOC compared to two doses of vaccine. Information on the extent and duration of viral shedding from vaccinated individuals infected with Omicron VOC is currently missing or very preliminary.
Due to the limited data on vaccine effectiveness against severe disease caused by Omicron VOC, it is not yet possible to draw conclusions based on real-life data.
Data from South Africa have recently shown a 70% (95% CI: 62-76%) vaccine effectiveness against hospitalisation during the Omicron period compared to the 93% (95% CI: 90-94%) observed in the pre-Omicron period [REF]. A UK study that examined association between both variant and vaccination status and risk of hospitalisation estimated a vaccine effectiveness against hospitalisation of 88% (78 to 93%) for Omicron after three doses of vaccine.
A recent preprint has also shown for Comirnaty and Janssen COVID-19 vaccine (that use two different technology platforms) broad cross-reactive cellular immunity against all variants, including Omicron. As cellular immunity is considered important, particularly for the protection against severe COVID-19 disease, the expectation is that vaccine effectiveness against severe disease should be somewhat reduced, but higher and more sustained than the one observed for infection and symptomatic disease due to Omicron.
It is important to consider that vaccine effectiveness is a relative measure (risk of hospitalisation due to Omicron VOC among vaccinated individuals compared to the risk among unvaccinated individuals) and should be interpreted in the light of the baseline severity of the Omicron VOC compared to the baseline severity of the previous variants. Preliminary data are in fact suggesting a two-thirds reduction in hospitalisations with the Omicron VOC compared to the Delta VOC.
Overall level of risk and options for response
Based on the current situation and the available evidence, ECDC’s Rapid Risk Assessment 18th Update on the impact of Omicron remains valid: the overall level of risk to public health associated with the further emergence and spread of the SARS-CoV-2 Omicron VOC in the EU/EEA is assessed as VERY HIGH.
Over the coming weeks, the very high growth advantage of Omicron is expected to result in even higher overall case notification rates. Such high levels of SARS-CoV-2 transmission may lead to high levels of absence from work including among healthcare and other essential workers and are likely to overwhelm the testing and contact tracing capacities in many EU Member States. The sheer volume of COVID-19 cases anticipated to occur are expected to place considerable strain on healthcare systems and society.
Please see the ECDC’s Rapid Risk Assessment for epidemiological forecasts and options for response (non-pharmaceutical interventions, health system strengthening, vaccination, testing and contact tracing, and risk communication). ECDC will publish updates on the epidemiological situation, severity, spread, and vaccine effectiveness in short intervals.
Awaiting further evidence becoming available, an urgent and strong action is needed to reduce transmission, keep the burden on healthcare systems manageable, and protect the most vulnerable in the coming months.
Member States should urgently assess their acceptable levels of residual risks, current healthcare system capacities, and available risk management options (e.g. contingency and business continuity measures, surveillance and testing strategy, quarantine and isolation policy, etc.).
Strengthening of non-pharmaceutical interventions is necessary to reduce ongoing Delta VOC and Omicron VOC transmission and keep the COVID-19-related disease burden manageable. These measures include avoiding large public or private gatherings, extended use of face masks, reduced contacts between groups of individuals in social or work settings, teleworking, and reduced inter-household mixing.
Vaccination remains a key component of the multi-layered approach needed to address the ongoing circulation and reduce the impact of the Delta and Omicron VOCs. Efforts should continue to increase full vaccination uptake in individuals who are currently unvaccinated or partially vaccinated and accelerate the roll-out of booster doses.
Member States are strongly encouraged to conduct and share findings on outbreak investigations and epidemiological studies to inform future risk assessments.