Healthcare-associated infections in intensive care units - Annual Epidemiological Report for 2017
Take our survey
Share your feedback in our short survey and help us improve publications at ECDC. Your input is valuable!
This report is based on data for 2017 retrieved from The European Surveillance System (TESSy) on 26 April 2019. TESSy is a system for the collection, analysis and dissemination of data on communicable diseases. EU Member States and EEA countries contribute to the system by uploading their infectious disease surveillance data at regular intervals.
Executive Summary
Key facts:
- In 2017, 8.3% (11 787) of the patients who stayed in intensive-care units (ICUs) for more than two days presented with at least one ICU-acquired healthcare-associated infection (HAI) under surveillance (pneumonia, bloodstream infection, or urinary tract infection).
- Of all patients staying in an ICU for more than two days, 6% presented with pneumonia, 4% with bloodstream infection (BSI), and 2% with urinary tract infection (UTI).
- Ninety-seven per cent of pneumonia episodes were associated with intubation, 37% of BSI episodes were catheter-related, and 98% of UTI episodes were associated with presence of a urinary catheter.
- The most frequently isolated microorganism was Pseudomonas aeruginosa in ICU-acquired pneumonia episodes, coagulase-negative staphylococci in ICU-acquired BSIs, and Esc herichia coli in ICU-acquired UTIs.
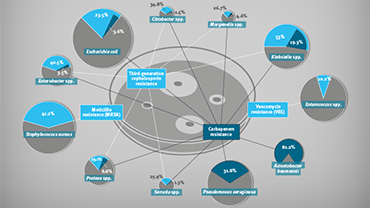
- Twenty-four per cent of Staphylococcus aureus isolates were oxacillin-resistant (MRSA) and 10% of Enterococcus spp. were glycopeptide resistant. Resistance to third-generation cephalosporins was reported in 16% of E. coli isolates, 40% of Klebsiella spp. isolates and 34% of Enterobacter spp. isolates. Carbapenem resistance was reported in 15% of Klebsiella spp. isolates, 26% of P. aeruginosa isolates and 64% of Acinetobacter baumannii isolates.