Interim public health considerations for COVID-19 vaccination of children aged 5-11 years
Take our survey
Share your feedback in our short survey and help us improve publications at ECDC. Your input is valuable!
This technical report provides a set of interim public health considerations to support EU/EEA public health authorities taking decisions on the administration of COVID-19 vaccines to children aged 5-11 years.
Executive Summary
Key messages
- Surveillance data show that children aged 5-11 years have made up an increasing proportion of both notified cases and hospitalisations in EU/EEA countries in recent months. Although hospitalisations have increased in line with case rates in all age groups in the EU/EEA, disease severity of COVID-19 in children is generally mild with a favourable clinical outcome. Severe COVID-19 remains rare among children (of 65 800 notified symptomatic COVID-19 cases in children aged 5-11 years, reported from 10 EU/EEA countries during the period of B.1.617.2 (Delta) variant of concern (VOC) dominance, 0.61% were hospitalised and 0.06% needed intensive care unit (ICU)/respiratory support).
- The relative contribution of children to overall SARS-CoV-2 circulation may have increased due to factors including the emergence of the highly transmissible Delta VOC and increased vaccination coverage in older age groups.
- The presence of an underlying condition among children aged 5-11 years is associated with about 12 times higher odds of hospitalisation and 19 times higher odds or of ICU admission. However, the majority (78%) of hospitalised children of this age had no reported underlying medical condition.
- Paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2/multi-inflammatory syndrome in children (PIMS-TS/MIS-C) and post COVID-19 condition have been reported in children aged 5-11 years, although it is difficult to quantify the prevalence and burden of these conditions. In a United States (US) Centers for Disease Control and Prevention (CDC) report, myocarditis was reported up to 37 times more often in unvaccinated children less than 16 years old with a COVID-19 diagnosis compared to other patients from the same age group.
- Beyond the direct health impacts of COVID-19 disease, the COVID-19 pandemic has affected the physical and mental health and well-being of children aged 5-11 years. Numerous factors, such as disruptions to important everyday social and educational activities, have caused anxiety and distress in this age group.
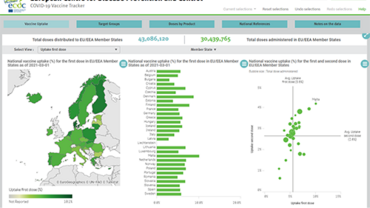
- Modelling data indicate that vaccinating children aged 5-11 years could reduce SARS-CoV-2 transmission in the whole population, although the extent and duration of this protection is currently unknown. It is estimated that the impact on the effective reproduction number (??) in the population as a whole would be a decrease of 11% (range: 8-15%, depending on vaccine uptake parameters of 30-70%) for an average country in the EU/EEA. This is comparable to the effect of some non-pharmaceutical interventions. The impact of vaccinating children is weaker for countries with a low adult vaccine uptake and stronger for countries with high uptake among adults.
- On 25 November 2021, the European Medicines Agency (EMA) granted a positive opinion for use of the Comirnaty COVID-19 vaccine in children aged 5-11 years based on a placebo-controlled randomised clinical trial in which more than 3 000 children in this age group received this vaccine.
- Children aged 5-11 years who are at risk of severe COVID-19 should be considered a priority group for vaccination against COVID-19, as in other age groups. However, since hospitalisation, PIMS-TS/MIS-C and post COVID-19 condition can also occur among children with no known risk factors, consideration could be given to the vaccination of all children aged 5-11 years.
- COVID-19 vaccine safety data in children aged 5-11 years are currently limited, and the level of natural immunity in the unvaccinated and its duration are currently unknown and likely heterogeneous across the population.
- The main priority of COVID-19 vaccination campaigns seeking to reduce COVID-19-related morbidity and mortality remains to increase vaccine uptake in the eligible adult population. Before taking policy decisions on COVID-19 vaccination in children, potential harms and benefits – including the direct and indirect effects on health and well-being – should be considered alongside the vaccine uptake and epidemiological situation in a particular country. Aspects around implementation and health equity should also be taken into consideration.