Rapid risk assessment: Hospital-acquired malaria infections in the European Union
Following the occurrence of several hospital-acquired malaria cases in the European Union (EU), ECDC has assessed the risk related to transmission of the parasite in hospital settings.
Executive Summary
Between January 2016 and April 2018, six sporadic hospital transmissions of malaria were identified in the European Union (EU). Although uncommon, hospital transmission of malaria has been described previously. While the countries reporting these six cases (i.e. Germany, Greece, Italy and Spain) have not observed an increase in the number of sporadic hospital-acquired cases of malaria since January 2016, the concomitant occurrence of these cases in four countries makes the overall event unusual. The mode(s) of transmission have not been determined for any of the cases. This rapid risk assessment presents the context, details investigations into the cases and offers options for prevention and control.
According to the scientific literature, the following modes of transmission should be taken into account in the investigation of hospital-acquired malaria:
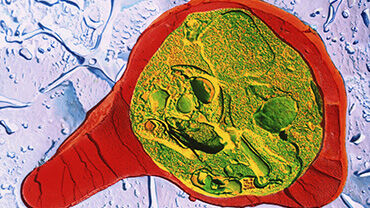
- Parenteral introduction of blood that contains parasite-infected erythrocytes from one infectious individual to another patient during healthcare procedures;
- Blood transfusion, or bone marrow or organ transplant from a malaria-infected patient;
- Accidental contact of blood containing parasite-infected erythrocytes with an open wound.
Malaria transmission in a hospital can also be vector-borne, when a malaria-infected mosquito bites a hospitalised patient. According to the literature, investigations are not always conclusive and entomological investigations may fail to identify rare events of vector-borne transmission such as transmission in hospital settings, airport malaria or luggage malaria.
Clinicians must be aware of the possibility of hospital-acquired malaria in hospitalised or recently discharged patients who develop an unexplained fever or a malaria-like clinical syndrome, especially if their hospital admission coincided with that of another patient admitted with malaria.
Healthcare providers should be aware that hospital transmission of malaria is rare but possible, irrespective of the Plasmodium species involved. However, hospital transmission has almost always been associated with P. falciparum . Patients with malaria should always be considered infectious by the parenteral route.
Prevention of transmission in hospitals requires that standard precautions are strictly implemented, including safe injection practices that prevent the sharing of patient care devices or equipment which may be contaminated by patient blood. Transmission of blood-borne pathogens is linked to the sharing of glucose monitoring, capillary blood sampling or insulin administration devices, multi-dose vials, or single-use ampoules among patients and the failure to change gloves after handling intravascular catheters or performing capillary blood testing. Reusable patient care equipment should be cleaned and disinfected between patients in accordance with manufacturer’s instructions. The sharing of multi-dose vials among patients should be avoided. If it is necessary to share, a sterile syringe and sterile needle must be used each time the multi-dose vial is accessed.
An investigation and assessment of infection prevention and control procedures and practices related to bloodborne transmission is indicated in the event of any suspected hospital transmission of malaria (e.g. handling of intravascular catheters, capillary blood sampling, use of glucometers, use of multi-dose drug vials, saline and heparin flushes, and use of gloves.) Investigations should also include an assessment of possible transmission through blood transfusion, bone marrow or organ transplantation, concurrent with a malaria case in the hospital, an assessment of possible vector-borne transmission by a local vector or associated with travel in a malaria-endemic country, airport/harbour or luggage malaria, and molecular typing of Plasm odium spp. isolates (when possible).
If a high local vector capacity supports increased risk of vector-borne transmission, prevention measures should be considered to avoid patients or personnel being bitten by mosquitoes (e.g. bed-nets, insect repellents) when a patient with malaria is hospitalised.
The risk of further spread of malaria in the EU associated with these recent events is considered negligible.
Competent authorities are encouraged to report new human cases of hospital transmission of malaria and the findings of public health investigations to the Epidemic Intelligence Information System for Antimicrobial Resistance and Healthcare-associated Infections (EPIS-AMR-HAI). Where appropriate, competent public health authorities are encouraged to issue notifications on EWRS, as per Article 9 of Decision 1082/2013/EU on serious cross-border threats to health.
Download

Erratum – on 3 May 2018 in paragraph 2, page 5 (section on Greece), the words ‘another facility’ were replaced with ‘the same hospital’. First part of sentence now reads: ‘The case, with no recent travel history to a malaria-endemic area, had previously been hospitalised in the same hospital between 17 June and 10 July 2018…’